Histoplasmosis is a fungal infection caused by inhaling spores of Histoplasma capsulatum, commonly found in bird and bat droppings. Symptoms can range from mild respiratory issues to severe lung complications, especially in immunocompromised individuals. Discover more about the causes, symptoms, and treatment options to protect Your health in the full article.
Table of Comparison
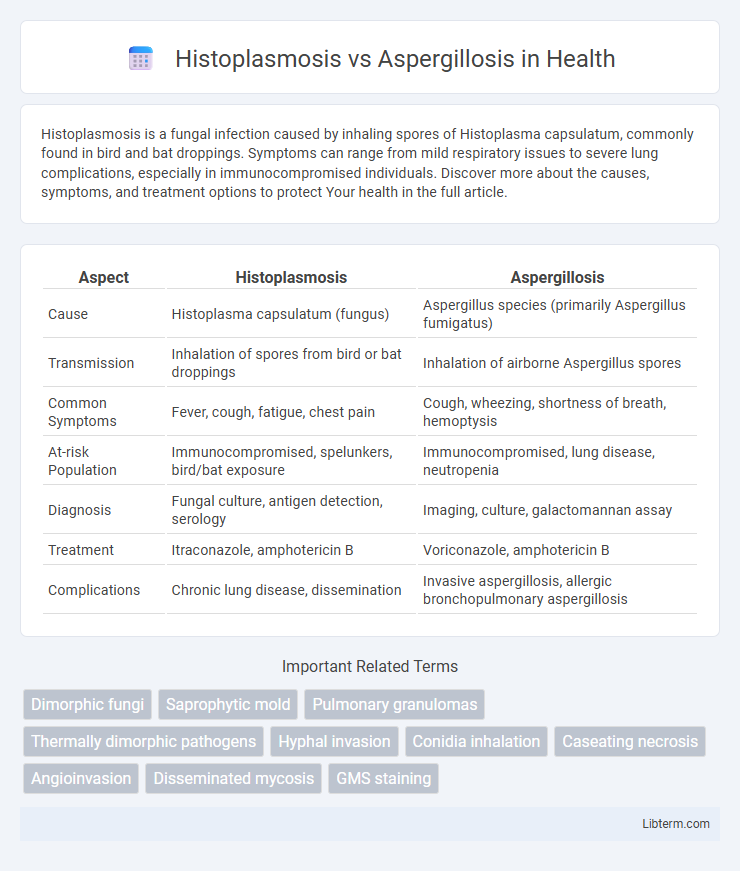
| Aspect | Histoplasmosis | Aspergillosis |
|---|---|---|
| Cause | Histoplasma capsulatum (fungus) | Aspergillus species (primarily Aspergillus fumigatus) |
| Transmission | Inhalation of spores from bird or bat droppings | Inhalation of airborne Aspergillus spores |
| Common Symptoms | Fever, cough, fatigue, chest pain | Cough, wheezing, shortness of breath, hemoptysis |
| At-risk Population | Immunocompromised, spelunkers, bird/bat exposure | Immunocompromised, lung disease, neutropenia |
| Diagnosis | Fungal culture, antigen detection, serology | Imaging, culture, galactomannan assay |
| Treatment | Itraconazole, amphotericin B | Voriconazole, amphotericin B |
| Complications | Chronic lung disease, dissemination | Invasive aspergillosis, allergic bronchopulmonary aspergillosis |
Overview of Histoplasmosis and Aspergillosis
Histoplasmosis is a fungal infection caused by Histoplasma capsulatum, primarily affecting the lungs after inhaling spores from bird or bat droppings in endemic regions like the Ohio and Mississippi River valleys. Aspergillosis results from Aspergillus species, particularly Aspergillus fumigatus, leading to a spectrum of respiratory conditions ranging from allergic reactions to invasive lung disease, especially in immunocompromised individuals. Both infections require prompt diagnosis through imaging and laboratory cultures to guide antifungal treatment strategies.
Causative Fungi: Histoplasma vs Aspergillus
Histoplasmosis is caused by the dimorphic fungus Histoplasma capsulatum, which thrives in soil enriched with bird or bat droppings, particularly in endemic regions like the Ohio and Mississippi River valleys. Aspergillosis results from Aspergillus species, primarily Aspergillus fumigatus, a ubiquitous mold found in decaying organic matter and indoor environments with high spore counts. Both fungi lead to pulmonary infections but differ significantly in habitat, morphology, and disease pathogenesis, influencing diagnosis and treatment strategies.
Modes of Transmission and Risk Factors
Histoplasmosis transmits primarily through inhalation of spores from soil contaminated with bird or bat droppings, commonly affecting individuals exposed to caves, old buildings, or poultry farms. Aspergillosis occurs via inhalation of airborne Aspergillus spores, frequently present in decaying vegetation, compost, or dust, posing higher risk to immunocompromised patients and those with lung diseases. Both diseases disproportionately impact individuals with weakened immune systems, but histoplasmosis is more associated with environmental exposure in endemic regions, while aspergillosis is linked to hospital settings and agricultural environments.
Geographic Distribution and Epidemiology
Histoplasmosis primarily occurs in the Ohio and Mississippi River valleys in the United States, with endemic regions extending to parts of Central and South America, Africa, and Asia, where soil enriched with bird or bat droppings favors fungal growth. Aspergillosis, caused by Aspergillus species, has a worldwide distribution but is more prevalent in environments with decaying organic matter, affecting immunocompromised individuals globally without specific geographic restriction. Epidemiologically, histoplasmosis often presents as localized outbreaks linked to environmental exposure, whereas aspergillosis generally manifests as sporadic cases associated with hospital settings and patients with weakened immune defenses.
Clinical Manifestations: Similarities and Differences
Histoplasmosis and aspergillosis both primarily affect the respiratory system, presenting with symptoms such as cough, fever, and chest pain, but histoplasmosis often manifests with acute or chronic pulmonary infections and may mimic tuberculosis. Aspergillosis exhibits a broader spectrum, including allergic bronchopulmonary aspergillosis, chronic pulmonary aspergillosis, and invasive aspergillosis, especially in immunocompromised patients, with symptoms ranging from wheezing and hemoptysis to severe systemic infection. Fever and respiratory distress are common in both, but aspergillosis more frequently leads to angioinvasion and tissue necrosis, complicating clinical outcomes.
Diagnostic Approaches for Each Infection
Histoplasmosis diagnosis primarily relies on fungal culture, histopathology, and antigen detection tests in urine or serum, with PCR assays offering rapid identification of Histoplasma capsulatum DNA. Aspergillosis diagnosis involves imaging techniques like CT scans to detect characteristic lung lesions, combined with microbiological methods such as culture, galactomannan antigen testing, and PCR for Aspergillus DNA in respiratory samples. Serological tests are less reliable for aspergillosis compared to histoplasmosis, emphasizing the importance of integrating clinical, radiological, and laboratory data for accurate differentiation.
Imaging Findings in Histoplasmosis vs Aspergillosis
Histoplasmosis imaging often reveals diffuse micronodular or reticulonodular patterns along with mediastinal lymphadenopathy and calcified granulomas, while aspergillosis typically presents with cavitary lesions, nodules with a halo sign, or air crescent sign on chest CT. Histoplasmosis may demonstrate a more diffuse interstitial pattern due to granulomatous inflammation, contrasting with the angioinvasive nature of aspergillosis that leads to focal lung necrosis and hemorrhage seen as nodular consolidations. Imaging differentiation is critical for diagnosis, as histoplasmosis is linked to endemic areas with soil exposure, whereas aspergillosis primarily affects immunocompromised patients.
Treatment Strategies and Drug Choices
Treatment strategies for histoplasmosis primarily involve antifungal agents such as itraconazole for mild to moderate cases and amphotericin B for severe or disseminated infections. Aspergillosis management depends on the clinical form, with voriconazole as the first-line treatment for invasive aspergillosis and surgical intervention often necessary for chronic forms. Both infections require careful monitoring of drug levels and potential toxicity, given the prolonged therapy duration and the patient's immune status.
Prognosis and Potential Complications
Histoplasmosis prognosis varies, often resolving without treatment in immunocompetent individuals but causing severe disseminated disease in immunocompromised patients, with complications including chronic pulmonary fibrosis and adrenal insufficiency. Aspergillosis prognosis depends on the form; invasive aspergillosis carries high mortality, especially in neutropenic or transplant patients, and complications can include angioinvasion leading to hemorrhage and disseminated infection. Both fungal infections require timely antifungal therapy to mitigate risks of chronic disease, respiratory failure, and systemic spread.
Prevention and Public Health Considerations
Prevention of histoplasmosis centers on minimizing exposure to environments contaminated with bird or bat droppings, using protective equipment during activities like cave exploration or demolition, and implementing public health measures to control endemic areas. Aspergillosis prevention emphasizes reducing exposure to airborne Aspergillus spores through improved air filtration, especially in healthcare settings, and vigilant monitoring of immunocompromised individuals at higher risk. Public health strategies for both infections include raising awareness about occupational hazards, enhancing diagnostic capabilities, and promoting early intervention to reduce morbidity and healthcare costs.
Histoplasmosis Infographic
 libterm.com
libterm.com