Angiotensin plays a crucial role in regulating blood pressure by constricting blood vessels and stimulating the release of aldosterone, which controls salt and water balance in the body. Dysfunction or imbalances in the angiotensin system can contribute to hypertension and cardiovascular diseases. Explore this article to understand how angiotensin affects your health and the latest treatments targeting this vital hormone.
Table of Comparison
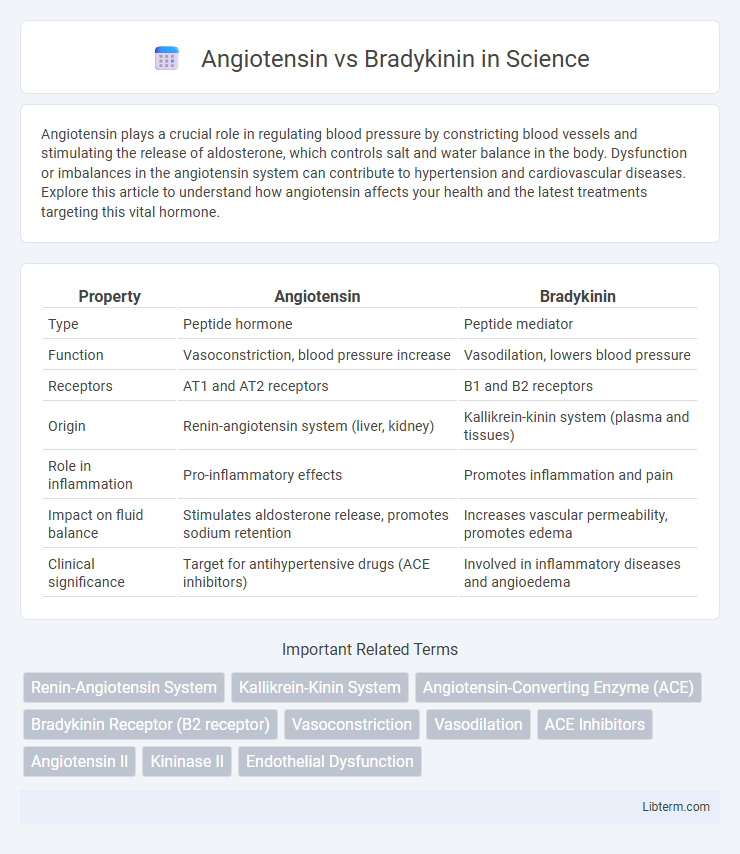
| Property | Angiotensin | Bradykinin |
|---|---|---|
| Type | Peptide hormone | Peptide mediator |
| Function | Vasoconstriction, blood pressure increase | Vasodilation, lowers blood pressure |
| Receptors | AT1 and AT2 receptors | B1 and B2 receptors |
| Origin | Renin-angiotensin system (liver, kidney) | Kallikrein-kinin system (plasma and tissues) |
| Role in inflammation | Pro-inflammatory effects | Promotes inflammation and pain |
| Impact on fluid balance | Stimulates aldosterone release, promotes sodium retention | Increases vascular permeability, promotes edema |
| Clinical significance | Target for antihypertensive drugs (ACE inhibitors) | Involved in inflammatory diseases and angioedema |
Introduction to Angiotensin and Bradykinin
Angiotensin is a peptide hormone crucial in regulating blood pressure and fluid balance by constricting blood vessels and stimulating aldosterone release. Bradykinin, a potent vasodilator peptide, facilitates blood pressure reduction through the relaxation of vascular smooth muscles and increased vascular permeability. Both molecules play opposing roles in cardiovascular homeostasis, influencing the renin-angiotensin system and the kallikrein-kinin system, respectively.
Overview of the Renin-Angiotensin System
The Renin-Angiotensin System (RAS) plays a crucial role in regulating blood pressure and fluid balance by converting angiotensinogen into angiotensin II, a potent vasoconstrictor that increases blood pressure. Bradykinin, a peptide degraded by angiotensin-converting enzyme (ACE), promotes vasodilation and lowers blood pressure, counterbalancing the effects of angiotensin II. The interaction between angiotensin II and bradykinin within the RAS modulates vascular tone and contributes to cardiovascular homeostasis.
Biosynthesis and Functions of Angiotensin
Angiotensin is synthesized from angiotensinogen, a liver-produced protein, through enzymatic actions involving renin and angiotensin-converting enzyme (ACE), leading to active peptides like angiotensin II. Angiotensin II functions as a potent vasoconstrictor, regulating blood pressure and stimulating aldosterone secretion to maintain electrolyte balance. In contrast, bradykinin is generated from kininogens by kallikreins and primarily induces vasodilation, opposing angiotensin's effects on vascular tone.
Bradykinin: Origin and Mechanism of Action
Bradykinin is a peptide produced from kininogen through the enzymatic action of kallikreins, primarily in response to tissue injury or inflammation. It exerts its effects by binding to B1 and B2 receptors on endothelial and smooth muscle cells, triggering vasodilation, increased vascular permeability, and pain sensation. This mechanism contrasts with angiotensin, which mainly promotes vasoconstriction and sodium retention through the angiotensin II pathway.
Comparative Molecular Structures
Angiotensin is an octapeptide primarily composed of hydrophobic and positively charged residues, facilitating strong receptor binding through specific angiotensin II receptor sites. Bradykinin, a nonapeptide, contains a higher proportion of hydrophilic amino acids and exhibits flexible conformations that promote its interaction with B1 and B2 receptors. The structural variance between angiotensin's rigid, receptor-specific conformation and bradykinin's flexible, receptor-diverse binding underpins their distinct physiological roles in vasoconstriction and vasodilation respectively.
Physiological Roles in Blood Pressure Regulation
Angiotensin primarily increases blood pressure through vasoconstriction and stimulating aldosterone release, which promotes sodium and water retention, enhancing blood volume. Bradykinin acts as a vasodilator by stimulating nitric oxide and prostacyclin production, leading to decreased blood pressure and improved vascular function. The balance between angiotensin's constrictive effects and bradykinin's dilatory influence is critical for maintaining vascular homeostasis and optimal blood pressure regulation.
Angiotensin vs Bradykinin: Effects on Vascular Tone
Angiotensin is a potent vasoconstrictor that increases vascular tone by stimulating smooth muscle contraction and promoting sodium retention, thereby elevating blood pressure. In contrast, Bradykinin acts as a vasodilator, reducing vascular tone through the release of nitric oxide and prostacyclin, which relax vascular smooth muscle and enhance blood flow. The opposing effects of Angiotensin and Bradykinin on vascular tone play critical roles in regulating blood pressure homeostasis and are targeted in therapies for hypertension and cardiovascular diseases.
Clinical Implications in Cardiovascular Diseases
Angiotensin plays a critical role in vasoconstriction and blood pressure regulation through the renin-angiotensin system, often contributing to hypertension and heart failure progression. Conversely, bradykinin acts as a potent vasodilator, promoting nitric oxide release and anti-inflammatory effects that protect endothelial function. Therapeutic modulation targeting angiotensin receptors or ACE inhibitors not only reduce angiotensin II levels but also increase bradykinin availability, offering dual benefits in managing cardiovascular diseases such as hypertension, atherosclerosis, and myocardial infarction.
Pharmacological Modulation and Therapeutic Applications
Angiotensin and bradykinin are key regulators in cardiovascular homeostasis, with angiotensin primarily mediating vasoconstriction through the angiotensin II type 1 receptor, while bradykinin induces vasodilation via B2 receptors. Pharmacological modulation of angiotensin involves ACE inhibitors and angiotensin receptor blockers (ARBs), which reduce hypertension and cardiac remodeling by inhibiting angiotensin II effects; conversely, ACE inhibitors increase bradykinin levels, enhancing its vasodilatory and cardioprotective actions but potentially causing side effects like cough. Therapeutic applications exploit this balance by targeting the renin-angiotensin-aldosterone system (RAAS) for managing hypertension, heart failure, and kidney diseases, leveraging bradykinin's beneficial vascular effects to improve outcomes.
Future Perspectives in Angiotensin and Bradykinin Research
Future perspectives in angiotensin and bradykinin research emphasize targeted therapies modulating the renin-angiotensin system and kallikrein-kinin system to treat cardiovascular diseases and inflammation more effectively. Advances in gene editing technologies like CRISPR and novel receptor-specific agonists or antagonists promise personalized medicine approaches, improving patient outcomes in hypertension and chronic inflammatory conditions. Ongoing studies aim to unravel complex signaling pathways and interactions, enabling innovative drug development with minimized side effects.
Angiotensin Infographic
 libterm.com
libterm.com