Granulation is a crucial process in pharmaceutical manufacturing that transforms powders into granules, improving flowability, compressibility, and uniformity for tablet and capsule production. This technique enhances dosage accuracy and ensures consistent drug delivery by controlling particle size and moisture content. Explore the following sections to understand how granulation impacts your medication's quality and effectiveness.
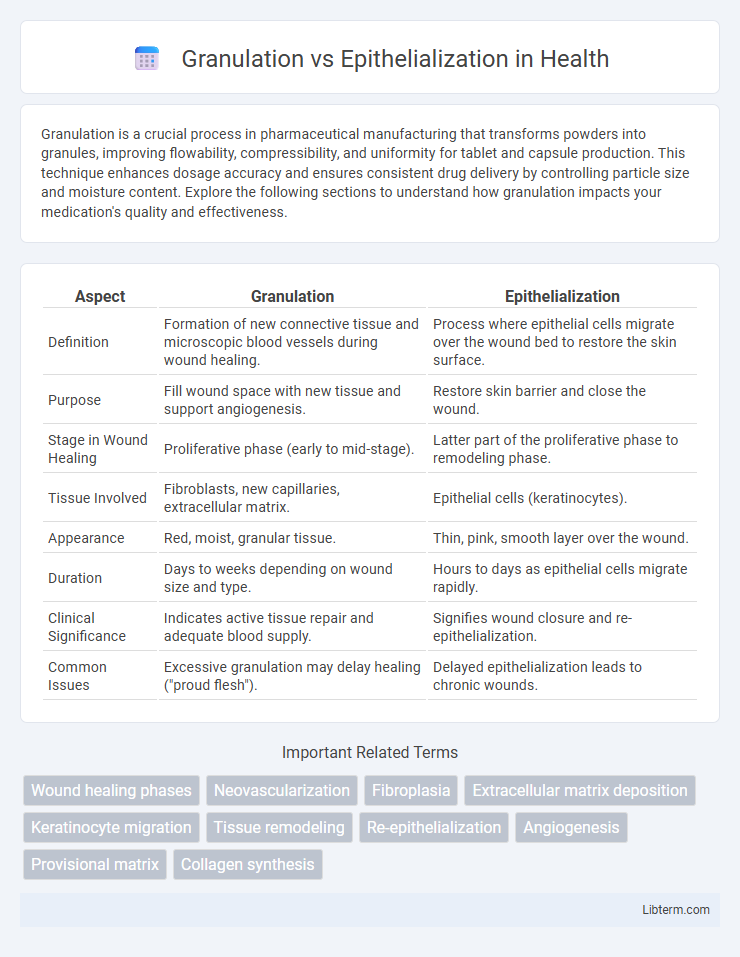
Table of Comparison
| Aspect | Granulation | Epithelialization |
|---|---|---|
| Definition | Formation of new connective tissue and microscopic blood vessels during wound healing. | Process where epithelial cells migrate over the wound bed to restore the skin surface. |
| Purpose | Fill wound space with new tissue and support angiogenesis. | Restore skin barrier and close the wound. |
| Stage in Wound Healing | Proliferative phase (early to mid-stage). | Latter part of the proliferative phase to remodeling phase. |
| Tissue Involved | Fibroblasts, new capillaries, extracellular matrix. | Epithelial cells (keratinocytes). |
| Appearance | Red, moist, granular tissue. | Thin, pink, smooth layer over the wound. |
| Duration | Days to weeks depending on wound size and type. | Hours to days as epithelial cells migrate rapidly. |
| Clinical Significance | Indicates active tissue repair and adequate blood supply. | Signifies wound closure and re-epithelialization. |
| Common Issues | Excessive granulation may delay healing ("proud flesh"). | Delayed epithelialization leads to chronic wounds. |
Understanding Wound Healing: Granulation vs Epithelialization
Granulation involves the formation of new connective tissue and microscopic blood vessels on the surface of a wound, providing a foundation for further healing. Epithelialization is the process where epithelial cells migrate across the granulated tissue, covering the wound and restoring the skin barrier. Understanding these phases is crucial for effective wound management and optimizing tissue regeneration.
Defining Granulation Tissue in Wound Repair
Granulation tissue is a specialized connective tissue essential for wound repair, characterized by the proliferation of new capillaries, fibroblasts, and extracellular matrix components. It forms the foundation for re-epithelialization by providing a vascularized and supportive environment that facilitates keratinocyte migration and wound closure. The presence of granulation tissue indicates active healing, promoting tissue regeneration and protecting the wound from infection.
The Role of Epithelialization in Healing
Epithelialization plays a critical role in wound healing by restoring the skin barrier through the migration and proliferation of epithelial cells over the wound bed. This process seals the wound, preventing infection and fluid loss, and facilitates the formation of a new protective layer. Unlike granulation, which primarily involves the formation of new connective tissue and blood vessels, epithelialization completes the healing process by covering the previously formed granulation tissue.
Cellular Mechanisms of Granulation
Granulation involves fibroblast proliferation and extracellular matrix deposition, primarily collagen, driven by growth factors such as platelet-derived growth factor (PDGF) and transforming growth factor-beta (TGF-b). Angiogenesis is stimulated by vascular endothelial growth factor (VEGF), promoting new capillary formation within the granulation tissue. In contrast, epithelialization depends on keratinocyte migration and proliferation to restore the epidermal barrier.
Epithelialization: Key Cells and Processes
Epithelialization involves keratinocytes migrating across the wound bed to restore the epidermal layer, playing a crucial role in wound closure. Key cells include keratinocytes, which proliferate and differentiate, and Langerhans cells that contribute to immune defense. The process depends on growth factors such as EGF (Epidermal Growth Factor) and TGF-b (Transforming Growth Factor-beta) to regulate cell migration, proliferation, and extracellular matrix remodeling essential for restoring skin integrity.
Granulation Phase: Signs and Characteristics
The granulation phase is marked by the formation of new connective tissue and microscopic blood vessels at the wound site, creating a granular tissue appearance. Key signs include a red or pink color indicating high vascularization, a moist and bumpy texture, and the presence of fibroblasts and macrophages that facilitate tissue regeneration and infection control. This phase is critical for laying down the extracellular matrix and collagen, essential for subsequent epithelialization and wound closure.
Epithelialization Phase: Visual Indicators
The epithelialization phase is characterized by the appearance of new, pinkish, and shiny epithelial tissue at the wound edges, signaling the formation of a protective barrier. Visual indicators include a smooth, moist surface and a reduction in wound size as keratinocytes migrate across the wound bed. Unlike granulation tissue, which appears red and bumpy due to new capillary growth, epithelialization presents a more translucent, thin layer indicative of skin regeneration.
Clinical Importance: Granulation vs Epithelialization
Granulation tissue forms the foundation for wound healing by filling the wound bed with new connective tissue and capillaries, critical for preventing infection and enabling nutrient delivery. Epithelialization restores the skin barrier by migrating epithelial cells over the granulation tissue, essential for wound closure and protection against environmental contaminants. Clinically, monitoring granulation quality and epithelialization progress helps assess healing stages, guide treatment decisions, and predict outcomes in chronic and acute wounds.
Factors Affecting Granulation and Epithelialization
Granulation and epithelialization are crucial phases in wound healing influenced by multiple factors. Granulation is primarily affected by adequate oxygenation, presence of growth factors like VEGF, and a moist wound environment supporting fibroblast proliferation and extracellular matrix deposition. Epithelialization depends on the migration and proliferation of keratinocytes, which are optimized by a clean wound bed, minimal infection, and balanced moisture levels to facilitate effective skin barrier restoration.
Optimizing Treatment: Supporting Both Healing Stages
Granulation and epithelialization represent critical stages in wound healing, with granulation involving new connective tissue and blood vessel formation while epithelialization restores the skin surface. Optimizing treatment requires maintaining a moist wound environment, controlling infection, and providing nutrients essential for fibroblast activity and keratinocyte migration. Supporting both stages accelerates tissue repair and minimizes scarring, enhancing overall wound closure efficiency.
Granulation Infographic
 libterm.com
libterm.com