Hypervolemia occurs when there is an excessive accumulation of fluid in the blood, leading to increased blood volume and pressure on the cardiovascular system. This condition can result from heart failure, kidney disease, or excessive intravenous fluid administration and requires careful management to prevent complications like edema and hypertension. Explore the article to understand the causes, symptoms, and treatment options for hypervolemia to safeguard your health.
Table of Comparison
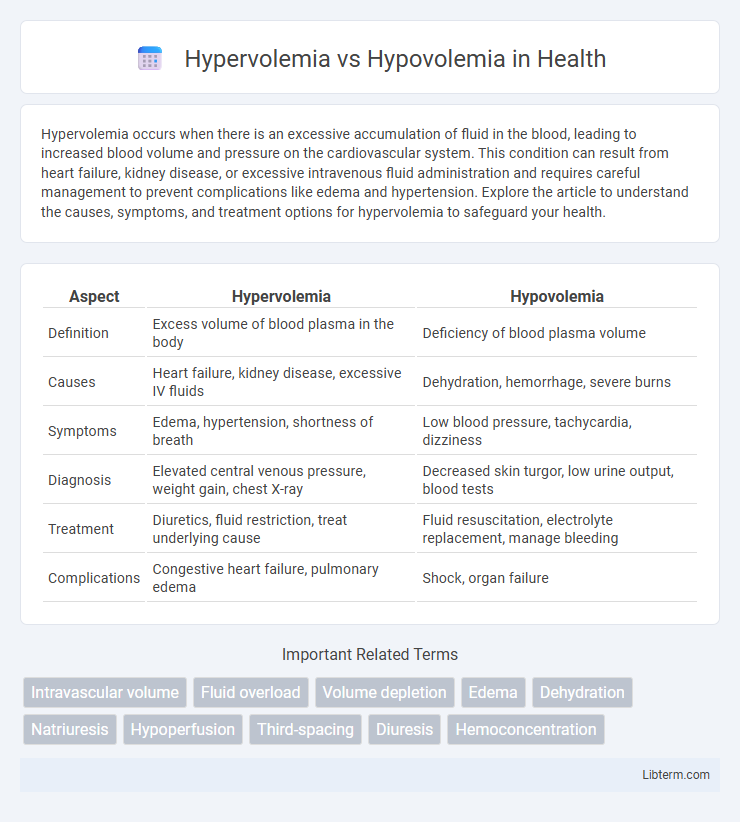
| Aspect | Hypervolemia | Hypovolemia |
|---|---|---|
| Definition | Excess volume of blood plasma in the body | Deficiency of blood plasma volume |
| Causes | Heart failure, kidney disease, excessive IV fluids | Dehydration, hemorrhage, severe burns |
| Symptoms | Edema, hypertension, shortness of breath | Low blood pressure, tachycardia, dizziness |
| Diagnosis | Elevated central venous pressure, weight gain, chest X-ray | Decreased skin turgor, low urine output, blood tests |
| Treatment | Diuretics, fluid restriction, treat underlying cause | Fluid resuscitation, electrolyte replacement, manage bleeding |
| Complications | Congestive heart failure, pulmonary edema | Shock, organ failure |
Introduction to Fluid Volume Disorders
Hypervolemia and hypovolemia represent opposite fluid volume imbalances affecting the body's extracellular fluid. Hypervolemia denotes excess fluid accumulation, often linked to conditions like heart failure, kidney disease, or liver cirrhosis, leading to edema and hypertension. Hypovolemia involves fluid deficit due to dehydration, hemorrhage, or severe burns, resulting in decreased blood volume, hypotension, and potential shock.
Defining Hypervolemia and Hypovolemia
Hypervolemia is defined as an excessive volume of fluid in the bloodstream, often resulting from conditions like heart failure, kidney disease, or excessive sodium intake, leading to edema and hypertension. Hypovolemia refers to a decreased volume of circulating blood plasma, commonly caused by hemorrhage, dehydration, or severe burns, resulting in hypotension and tachycardia. Both conditions disrupt fluid balance, impacting cardiovascular stability and requiring precise clinical management.
Causes of Hypervolemia
Hypervolemia, characterized by an excess of fluid in the blood vessels, often results from conditions such as congestive heart failure, chronic kidney disease, and excessive intravenous fluid administration. Sodium retention in disorders like cirrhosis and nephrotic syndrome also contributes to fluid overload by promoting water retention. In contrast, hypovolemia involves a significant loss of blood volume due to acute hemorrhage, dehydration, or severe burns, leading to decreased circulating blood volume.
Causes of Hypovolemia
Hypovolemia primarily results from excessive fluid loss due to hemorrhage, severe dehydration, or gastrointestinal losses such as vomiting and diarrhea. Other causes include third-spacing of fluids in conditions like burns or pancreatitis, and inadequate fluid intake in critically ill patients. Recognizing these underlying causes is essential for effective diagnosis and management of hypovolemic states.
Signs and Symptoms: Hypervolemia vs Hypovolemia
Hypervolemia presents with signs such as edema, hypertension, jugular venous distention, and tachycardia due to excess fluid volume in the bloodstream. Hypovolemia manifests through symptoms including hypotension, tachycardia, dry mucous membranes, decreased skin turgor, and rapid, weak pulse, indicating reduced circulating blood volume. Monitoring these contrasting clinical signs is essential for accurate diagnosis and effective management of fluid imbalances.
Diagnostic Criteria and Assessment
Hypervolemia is diagnosed through clinical signs such as peripheral edema, pulmonary congestion on chest X-ray, and increased central venous pressure, along with laboratory indicators including elevated brain natriuretic peptide (BNP) levels and reduced hematocrit. Hypovolemia assessment relies on identifying symptoms like hypotension, tachycardia, decreased skin turgor, and laboratory findings such as elevated blood urea nitrogen (BUN) to creatinine ratio and hemoconcentration. Both conditions require comprehensive evaluation using fluid balance charts, vital signs monitoring, and appropriate imaging to guide effective management.
Complications Associated with Fluid Imbalance
Hypervolemia can lead to complications such as pulmonary edema, hypertension, and congestive heart failure due to excessive fluid accumulation in the vascular system. Hypovolemia increases the risk of hypovolemic shock, acute kidney injury, and electrolyte imbalances caused by insufficient circulating blood volume. Both conditions disrupt homeostasis, resulting in compromised tissue perfusion and oxygen delivery.
Treatment Strategies for Hypervolemia
Treatment strategies for hypervolemia primarily involve fluid restriction and the use of diuretics such as loop diuretics to promote excess fluid excretion. Addressing the underlying cause, like heart failure or kidney disease, is crucial to prevent recurrence. In severe cases, dialysis may be required to remove excess fluid and electrolytes efficiently.
Treatment Approaches for Hypovolemia
Hypovolemia treatment primarily involves rapid fluid resuscitation using isotonic crystalloids like normal saline or lactated Ringer's solution to restore circulating blood volume and improve tissue perfusion. In cases of severe blood loss, blood transfusions or packed red blood cells may be necessary to correct anemia and maintain oxygen delivery. Close monitoring of vital signs, urine output, and laboratory parameters such as hematocrit and electrolytes guides ongoing management and prevents complications like shock or organ failure.
Prevention and Patient Education
Preventing hypervolemia involves careful monitoring of fluid intake and output, especially in patients with heart failure or renal disease, alongside educating patients to recognize early symptoms like swelling and shortness of breath. Hypovolemia prevention centers on adequate hydration, balanced electrolyte intake, and prompt management of conditions causing fluid loss such as vomiting, diarrhea, or excessive sweating. Patient education should emphasize the importance of reporting abnormal fluid retention or dehydration signs to healthcare providers for timely intervention.
Hypervolemia Infographic
 libterm.com
libterm.com