Nephrotic syndrome is a kidney disorder characterized by excessive protein loss in urine, leading to swelling, high cholesterol, and increased risk of infections. Understanding the causes, symptoms, and treatment options is essential for effectively managing this condition. Explore this article to learn how you can protect your kidney health and improve your quality of life.
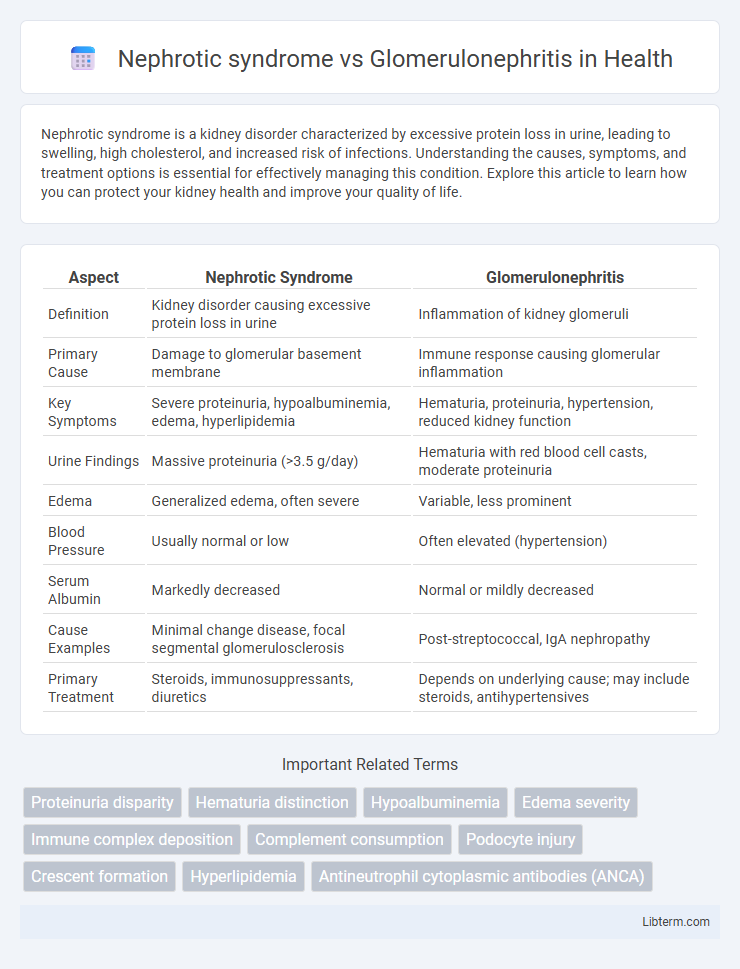
Table of Comparison
| Aspect | Nephrotic Syndrome | Glomerulonephritis |
|---|---|---|
| Definition | Kidney disorder causing excessive protein loss in urine | Inflammation of kidney glomeruli |
| Primary Cause | Damage to glomerular basement membrane | Immune response causing glomerular inflammation |
| Key Symptoms | Severe proteinuria, hypoalbuminemia, edema, hyperlipidemia | Hematuria, proteinuria, hypertension, reduced kidney function |
| Urine Findings | Massive proteinuria (>3.5 g/day) | Hematuria with red blood cell casts, moderate proteinuria |
| Edema | Generalized edema, often severe | Variable, less prominent |
| Blood Pressure | Usually normal or low | Often elevated (hypertension) |
| Serum Albumin | Markedly decreased | Normal or mildly decreased |
| Cause Examples | Minimal change disease, focal segmental glomerulosclerosis | Post-streptococcal, IgA nephropathy |
| Primary Treatment | Steroids, immunosuppressants, diuretics | Depends on underlying cause; may include steroids, antihypertensives |
Overview of Nephrotic Syndrome and Glomerulonephritis
Nephrotic syndrome is characterized by heavy proteinuria exceeding 3.5 grams per day, hypoalbuminemia, hyperlipidemia, and edema due to increased glomerular permeability. Glomerulonephritis involves inflammation and damage to the glomeruli, often presenting with hematuria, hypertension, and reduced renal function. Both conditions disrupt normal kidney filtration but differ in pathophysiology and clinical presentation, with nephrotic syndrome primarily causing protein loss and glomerulonephritis leading to inflammatory injury.
Key Differences in Pathophysiology
Nephrotic syndrome primarily results from podocyte injury leading to increased glomerular permeability and massive proteinuria, whereas glomerulonephritis involves inflammation of the glomeruli due to immune complex deposition or autoimmunity, causing hematuria and reduced glomerular filtration rate. The pathophysiology of nephrotic syndrome centers on the disruption of the glomerular filtration barrier, while glomerulonephritis features inflammatory cell infiltration and complement activation. These distinct mechanisms drive variations in clinical presentations, such as edema in nephrotic syndrome versus hypertension and renal impairment in glomerulonephritis.
Common Causes and Risk Factors
Nephrotic syndrome often results from minimal change disease, focal segmental glomerulosclerosis, or diabetic nephropathy, with risk factors including diabetes, infections, and certain medications. Glomerulonephritis primarily arises from autoimmune conditions like post-streptococcal infection, lupus nephritis, and IgA nephropathy, with key risk factors involving infections, systemic lupus erythematosus, and vasculitis. Both conditions share risk factors such as hypertension and chronic kidney disease but differ in their underlying immunologic and structural causes.
Clinical Manifestations: Signs and Symptoms
Nephrotic syndrome presents with massive proteinuria exceeding 3.5 grams per day, hypoalbuminemia, severe edema, and hyperlipidemia, often leading to foamy urine and pleural effusions. Glomerulonephritis typically manifests with hematuria, oliguria, hypertension, and mild to moderate proteinuria, accompanied by red blood cell casts in urine and azotemia. Both conditions may cause varying degrees of renal impairment, but nephrotic syndrome emphasizes protein loss and edema, while glomerulonephritis prominently features inflammation and hematuria.
Laboratory Findings and Diagnostic Criteria
Nephrotic syndrome is characterized by heavy proteinuria exceeding 3.5 grams per day, hypoalbuminemia, hyperlipidemia, and edema, with laboratory findings showing low serum albumin and elevated cholesterol levels. Glomerulonephritis presents with hematuria, usually dysmorphic red blood cells, variable proteinuria typically less than nephrotic range, and elevated serum creatinine indicating impaired kidney function, accompanied by active urine sediment with red blood cell casts. Diagnostic criteria for nephrotic syndrome emphasize quantitative proteinuria and hypoalbuminemia, while glomerulonephritis diagnosis relies on urinalysis for hematuria and red cell casts, serologic tests for underlying causes, and often kidney biopsy for definitive classification.
Histopathological Features
Nephrotic syndrome commonly exhibits diffuse podocyte foot process effacement and thickened glomerular basement membranes, often with minimal mesangial proliferation on histopathology. In contrast, glomerulonephritis typically shows mesangial hypercellularity, immune complex deposition, and variable degrees of glomerular inflammation and crescent formation. Electron microscopy and immunofluorescence are essential for distinguishing between these entities by revealing distinct patterns of immune deposits and structural alterations.
Complications and Prognostic Implications
Nephrotic syndrome commonly leads to complications such as severe proteinuria, hypoalbuminemia, edema, hyperlipidemia, and increased risk of thromboembolism and infections, which significantly affect morbidity. In contrast, glomerulonephritis often results in impaired renal function, hematuria, hypertension, and potential progression to chronic kidney disease or end-stage renal failure, posing a more direct threat to long-term renal prognosis. Prognostic outcomes vary with underlying etiology; nephrotic syndrome generally responds well to immunosuppressive therapy, whereas glomerulonephritis prognosis depends heavily on the specific subtype and timeliness of intervention.
Treatment Approaches and Management Strategies
Nephrotic syndrome treatment primarily involves corticosteroids like prednisone to reduce proteinuria and edema, alongside angiotensin-converting enzyme inhibitors (ACE inhibitors) or angiotensin receptor blockers (ARBs) to control blood pressure and minimize kidney damage. Glomerulonephritis management depends on the underlying cause but often includes immunosuppressive drugs such as corticosteroids and cyclophosphamide, blood pressure control with ACE inhibitors or ARBs, and sometimes plasmapheresis in severe cases. Both conditions require regular monitoring of kidney function, electrolyte balance, and protein levels to prevent progression to chronic kidney disease.
Long-Term Outcomes and Patient Prognosis
Nephrotic syndrome is characterized by heavy proteinuria, hypoalbuminemia, and edema, often leading to complications like chronic kidney disease and increased cardiovascular risk if untreated. Glomerulonephritis involves inflammation of the glomeruli, with long-term outcomes varying based on etiology but frequently resulting in progressive renal impairment or end-stage renal disease. Prognosis depends on early diagnosis, treatment adherence, and specific histopathological findings, with both conditions requiring close monitoring to prevent irreversible kidney damage.
Prevention Strategies and Patient Education
Preventing nephrotic syndrome and glomerulonephritis involves managing underlying conditions such as diabetes and infections that contribute to kidney damage. Patient education should emphasize adherence to prescribed medications, maintaining a low-sodium diet, and monitoring blood pressure regularly to reduce the risk of disease progression. Early detection through routine urine and blood tests plays a critical role in preventing complications associated with these kidney disorders.
Nephrotic syndrome Infographic
 libterm.com
libterm.com