Platelet aggregation is a crucial process in blood clot formation where platelets clump together to seal wounds and prevent excessive bleeding. This mechanism involves complex biochemical pathways and plays a vital role in cardiovascular health, influencing conditions such as heart attacks and strokes. Discover the detailed mechanisms and implications of platelet aggregation in the rest of this article.
Table of Comparison
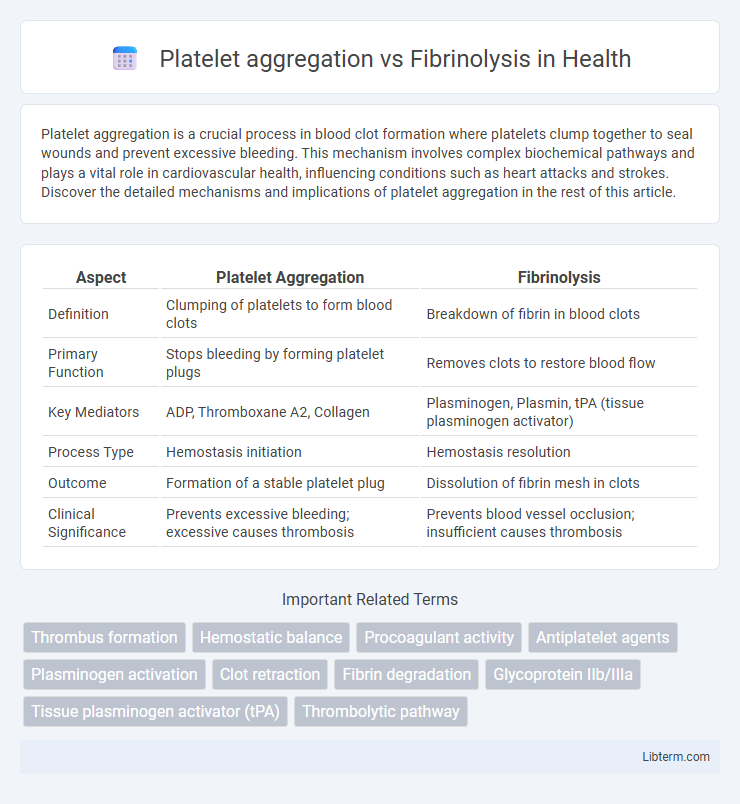
| Aspect | Platelet Aggregation | Fibrinolysis |
|---|---|---|
| Definition | Clumping of platelets to form blood clots | Breakdown of fibrin in blood clots |
| Primary Function | Stops bleeding by forming platelet plugs | Removes clots to restore blood flow |
| Key Mediators | ADP, Thromboxane A2, Collagen | Plasminogen, Plasmin, tPA (tissue plasminogen activator) |
| Process Type | Hemostasis initiation | Hemostasis resolution |
| Outcome | Formation of a stable platelet plug | Dissolution of fibrin mesh in clots |
| Clinical Significance | Prevents excessive bleeding; excessive causes thrombosis | Prevents blood vessel occlusion; insufficient causes thrombosis |
Introduction to Platelet Aggregation and Fibrinolysis
Platelet aggregation is a crucial initial step in hemostasis where activated platelets adhere to each other at sites of vascular injury, forming a primary platelet plug to prevent bleeding. Fibrinolysis, on the other hand, is the physiological process that breaks down fibrin clots through the action of plasmin, ensuring the removal of unnecessary clots and restoring normal blood flow. The balance between platelet aggregation and fibrinolysis maintains vascular integrity and prevents pathological thrombosis or excessive bleeding.
Mechanisms of Platelet Aggregation
Platelet aggregation is initiated by the activation of platelet surface receptors such as glycoprotein IIb/IIIa, which binds fibrinogen to cross-link platelets into a stable clot. This process involves the release of secondary messengers like ADP and thromboxane A2 that amplify platelet recruitment and activation at the injury site. In contrast, fibrinolysis is the enzymatic breakdown of fibrin clots primarily mediated by plasmin, serving to restore vascular patency after hemostasis.
Key Steps in Fibrinolysis
Fibrinolysis is a crucial biological process that breaks down fibrin clots to restore normal blood flow, initiated by the conversion of plasminogen to plasmin primarily catalyzed by tissue plasminogen activator (tPA) and urokinase. Plasmin enzymatically degrades the fibrin meshwork into soluble fibrin degradation products, effectively reversing platelet aggregation and clot formation. Regulation of fibrinolysis is tightly controlled by plasminogen activator inhibitors (PAI-1) and a2-antiplasmin to prevent excessive bleeding and maintain vascular integrity.
Major Molecules Involved in Platelet Aggregation
Platelet aggregation is primarily driven by molecules such as adenosine diphosphate (ADP), thromboxane A2 (TXA2), and glycoprotein IIb/IIIa receptors, which facilitate platelet activation and cross-linking. Fibrinolysis, in contrast, involves plasminogen activation to plasmin by tissue plasminogen activator (tPA) or urokinase, leading to fibrin clot degradation. Understanding the molecular players like fibrinogen binding to GP IIb/IIIa complexes highlights the interplay between platelet aggregation and fibrinolytic pathways in hemostasis.
Critical Enzymes Regulating Fibrinolysis
Plasminogen activators such as tissue plasminogen activator (tPA) and urokinase are critical enzymes regulating fibrinolysis by converting plasminogen into plasmin, which degrades fibrin clots. Inhibitors like plasminogen activator inhibitor-1 (PAI-1) modulate this process by preventing tPA and urokinase activity, balancing clot breakdown with platelet aggregation. The interplay between these enzymes ensures precise control over thrombus resolution and vascular homeostasis.
Platelet Aggregation in Hemostasis
Platelet aggregation is a crucial step in hemostasis, where platelets adhere to damaged blood vessel walls and clump together to form a primary platelet plug, preventing excessive blood loss. This process involves the activation of platelet surface receptors such as glycoprotein IIb/IIIa, which binds fibrinogen and stabilizes the platelet aggregate. In contrast, fibrinolysis is the physiological mechanism that dissolves blood clots by breaking down fibrin, ensuring the restoration of normal blood flow after vessel repair.
Fibrinolysis in Clot Resolution
Fibrinolysis plays a critical role in clot resolution by enzymatically breaking down fibrin networks that stabilize platelet aggregates during hemostasis. The key enzyme plasmin cleaves fibrin strands, facilitating the dissolution of the thrombus and restoring normal blood flow. This dynamic balance between platelet aggregation and fibrinolysis ensures effective clot formation to prevent bleeding, followed by timely clot removal to avoid vascular obstruction.
Pathological Conditions Related to Platelet Aggregation
Excessive platelet aggregation plays a critical role in pathological conditions such as thrombosis, leading to myocardial infarction, ischemic stroke, and deep vein thrombosis. Dysregulated platelet activation promotes arterial clot formation and vascular occlusion, contributing to atherosclerosis progression and acute coronary syndromes. Therapeutic targeting of platelet aggregation using antiplatelet agents reduces the risk of thrombotic events by balancing hemostasis and fibrinolysis processes.
Disorders Associated with Fibrinolytic Dysfunction
Disorders associated with fibrinolytic dysfunction primarily involve impaired clot breakdown, leading to conditions such as thrombosis, where excessive platelet aggregation disrupts normal blood flow. Hyperfibrinolysis results in excessive fibrin degradation, causing bleeding complications in diseases like liver cirrhosis or disseminated intravascular coagulation (DIC). Understanding the balance between platelet aggregation and fibrinolysis is crucial in managing thrombotic and hemorrhagic disorders effectively.
Therapeutic Modulation: Platelet Aggregation vs Fibrinolysis
Therapeutic modulation of platelet aggregation primarily involves the use of antiplatelet agents such as aspirin and P2Y12 inhibitors, which prevent thrombus formation by inhibiting platelet activation and aggregation pathways. In contrast, fibrinolysis is therapeutically targeted using fibrinolytic agents like tissue plasminogen activator (tPA) to promote the breakdown of fibrin clots, restoring blood flow in thrombotic events. Balancing the inhibition of platelet aggregation with the promotion of fibrinolysis is critical in managing cardiovascular diseases, stroke, and thromboembolic disorders while minimizing bleeding risks.
Platelet aggregation Infographic
 libterm.com
libterm.com