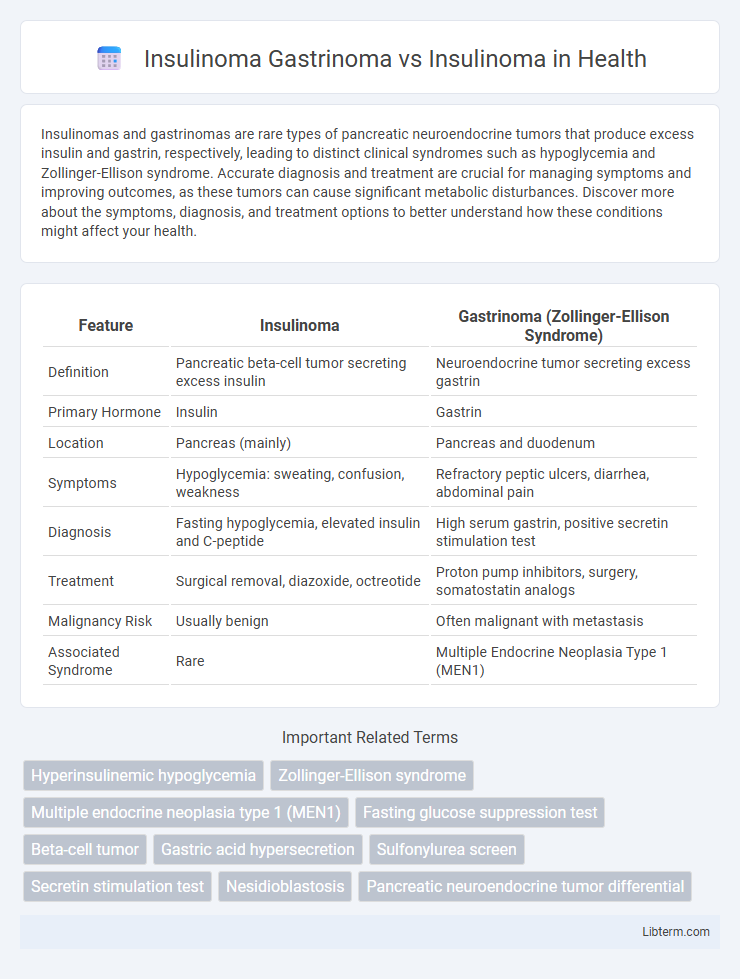
Insulinomas and gastrinomas are rare types of pancreatic neuroendocrine tumors that produce excess insulin and gastrin, respectively, leading to distinct clinical syndromes such as hypoglycemia and Zollinger-Ellison syndrome. Accurate diagnosis and treatment are crucial for managing symptoms and improving outcomes, as these tumors can cause significant metabolic disturbances. Discover more about the symptoms, diagnosis, and treatment options to better understand how these conditions might affect your health.
Table of Comparison
| Feature | Insulinoma | Gastrinoma (Zollinger-Ellison Syndrome) |
|---|---|---|
| Definition | Pancreatic beta-cell tumor secreting excess insulin | Neuroendocrine tumor secreting excess gastrin |
| Primary Hormone | Insulin | Gastrin |
| Location | Pancreas (mainly) | Pancreas and duodenum |
| Symptoms | Hypoglycemia: sweating, confusion, weakness | Refractory peptic ulcers, diarrhea, abdominal pain |
| Diagnosis | Fasting hypoglycemia, elevated insulin and C-peptide | High serum gastrin, positive secretin stimulation test |
| Treatment | Surgical removal, diazoxide, octreotide | Proton pump inhibitors, surgery, somatostatin analogs |
| Malignancy Risk | Usually benign | Often malignant with metastasis |
| Associated Syndrome | Rare | Multiple Endocrine Neoplasia Type 1 (MEN1) |
Introduction to Insulinoma and Gastrinoma
Insulinoma and gastrinoma are rare neuroendocrine tumors arising from the pancreas, each characterized by distinct hormone secretion profiles. Insulinomas primarily secrete insulin, leading to hypoglycemia, whereas gastrinomas produce excessive gastrin, causing Zollinger-Ellison syndrome with severe gastric acid hypersecretion. Both tumors require precise biochemical tests and imaging studies for diagnosis, with insulinomas often localized by endoscopic ultrasound and gastrinomas detected through fasting gastrin levels and somatostatin receptor imaging.
Key Differences Between Insulinoma and Gastrinoma
Insulinomas primarily secrete excessive insulin, causing hypoglycemia, whereas gastrinomas produce excessive gastrin, leading to Zollinger-Ellison syndrome with peptic ulcers and gastric acid hypersecretion. Insulinomas are typically small, solitary pancreatic tumors with benign behavior, while gastrinomas often present as multiple tumors, frequently located in the pancreas or duodenum, with a higher risk of malignancy. Diagnostic tests differ: insulinomas require supervised fasting and insulin/glucose ratio assessment, whereas gastrinomas are diagnosed via elevated fasting serum gastrin levels and gastric pH measurement.
Causes and Risk Factors of Insulinoma
Insulinoma primarily arises from pancreatic beta-cell tumors causing excessive insulin secretion, while gastrinoma originates from G-cells leading to increased gastrin production and Zollinger-Ellison syndrome. The main causes of insulinoma include sporadic mutations and genetic factors such as MEN1 (Multiple Endocrine Neoplasia type 1) syndrome, which significantly increases risk. Risk factors for insulinoma encompass a history of endocrine tumors, familial predisposition, and pancreatic neuroendocrine tumor development, distinguishing it from gastrinoma's association with acid hypersecretion-related complications.
Causes and Risk Factors of Gastrinoma
Gastrinomas primarily arise from neuroendocrine tumors in the pancreas or duodenum, causing excessive gastrin production leading to Zollinger-Ellison syndrome. The main causes of gastrinomas involve genetic mutations, such as those associated with multiple endocrine neoplasia type 1 (MEN1), which significantly increase the risk. Unlike insulinomas that secrete insulin and are usually sporadic, gastrinomas have a strong hereditary link and are influenced by factors like MEN1 and chronic gastritis.
Clinical Symptoms: Insulinoma vs Gastrinoma
Insulinomas primarily cause hypoglycemia symptoms such as confusion, sweating, palpitations, and seizures due to excessive insulin secretion. Gastrinomas typically present with recurrent peptic ulcers, abdominal pain, and diarrhea caused by elevated gastrin levels leading to gastric acid hypersecretion (Zollinger-Ellison syndrome). Differentiating clinical symptoms is crucial for diagnosis, with hypoglycemic episodes indicating insulinoma and acid-related gastrointestinal issues suggesting gastrinoma.
Diagnostic Approaches for Insulinoma and Gastrinoma
Diagnostic approaches for insulinoma primarily involve fasting tests to detect inappropriate insulin secretion during hypoglycemia, alongside imaging techniques such as endoscopic ultrasound and MRI to localize the tumor. Gastrinoma diagnosis relies on measuring elevated gastrin levels, particularly during secretin stimulation tests, combined with somatostatin receptor scintigraphy and cross-sectional imaging like CT or MRI to identify gastrin-secreting tumors. Both conditions benefit from selective arterial calcium stimulation tests to improve tumor localization accuracy when non-invasive methods prove inconclusive.
Biochemical Markers: Insulin vs Gastrin Levels
Insulinoma typically presents with markedly elevated insulin and C-peptide levels during hypoglycemia, confirming endogenous hyperinsulinism. Gastrinoma is characterized by significantly increased fasting gastrin concentrations, often exceeding ten times the upper normal limit, alongside elevated gastric acid output. Differentiation between insulinoma and gastrinoma relies on these distinct biochemical markers, with insulin and C-peptide indicating insulinoma and hypergastrinemia indicating gastrinoma.
Imaging Modalities in Differentiation
Imaging modalities play a crucial role in differentiating insulinoma from gastrinoma, with multiphasic contrast-enhanced CT scans and endoscopic ultrasound (EUS) providing high sensitivity for insulinomas due to their typically small size and pancreatic localization. Gastrinomas, often located in the duodenum or pancreas, are better identified using somatostatin receptor scintigraphy (SRS) and 68Ga-DOTATATE PET/CT, which target neuroendocrine tumor-specific receptors. MRI aids in soft tissue contrast, while selective arterial calcium stimulation with hepatic venous sampling enhances localization accuracy for both tumors in complex cases.
Treatment Options for Insulinoma and Gastrinoma
Treatment options for insulinoma primarily involve surgical resection, which is the most effective curative approach, especially for localized tumors, while medical therapies such as diazoxide and somatostatin analogs help manage hypoglycemia symptoms in inoperable cases. In contrast, gastrinoma treatment often requires a combination of surgery to remove the tumor and proton pump inhibitors or H2 receptor antagonists to control gastrin-induced acid hypersecretion and prevent peptic ulcers. For metastatic or unresectable gastrinomas, targeted therapies like somatostatin analogs and chemotherapy may be employed to control tumor growth and hormone secretion.
Prognosis and Patient Outcomes: A Comparative Overview
Insulinoma and gastrinoma, both neuroendocrine tumors of the pancreas, differ significantly in prognosis and patient outcomes, with insulinomas generally presenting a more favorable clinical course due to their typically benign nature and lower malignancy rate. Gastrinomas often exhibit a higher malignant potential, leading to Zollinger-Ellison syndrome and associated complications such as peptic ulcers and gastroesophageal reflux, which can complicate management and worsen prognosis. Early detection and surgical resection improve outcomes in insulinoma patients, whereas gastrinoma treatment requires a multidisciplinary approach including proton pump inhibitors and oncologic therapies to manage hormone hypersecretion and tumor progression.
Insulinoma Gastrinoma Infographic
 libterm.com
libterm.com