Gastroesophageal reflux disease (GERD) causes stomach acid to frequently flow back into the esophagus, leading to symptoms like heartburn, regurgitation, and difficulty swallowing. Persistent GERD can damage the esophageal lining and increase the risk of complications such as esophagitis and Barrett's esophagus. Discover effective treatments and lifestyle adjustments to manage your GERD by reading the rest of this article.
Table of Comparison
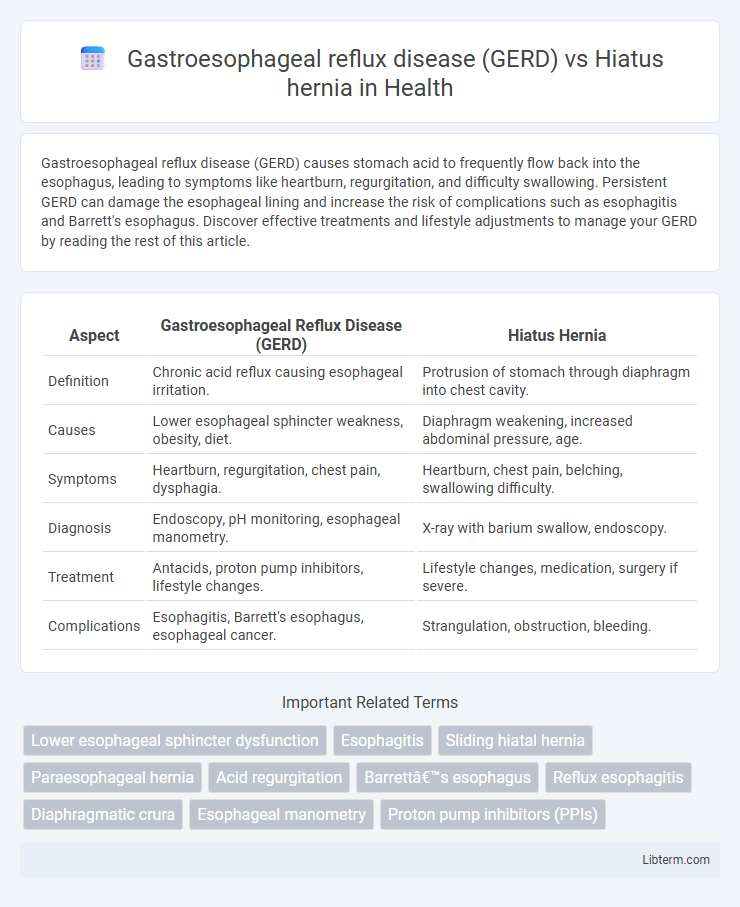
| Aspect | Gastroesophageal Reflux Disease (GERD) | Hiatus Hernia |
|---|---|---|
| Definition | Chronic acid reflux causing esophageal irritation. | Protrusion of stomach through diaphragm into chest cavity. |
| Causes | Lower esophageal sphincter weakness, obesity, diet. | Diaphragm weakening, increased abdominal pressure, age. |
| Symptoms | Heartburn, regurgitation, chest pain, dysphagia. | Heartburn, chest pain, belching, swallowing difficulty. |
| Diagnosis | Endoscopy, pH monitoring, esophageal manometry. | X-ray with barium swallow, endoscopy. |
| Treatment | Antacids, proton pump inhibitors, lifestyle changes. | Lifestyle changes, medication, surgery if severe. |
| Complications | Esophagitis, Barrett's esophagus, esophageal cancer. | Strangulation, obstruction, bleeding. |
Introduction to GERD and Hiatus Hernia
Gastroesophageal reflux disease (GERD) is a chronic condition characterized by the backflow of stomach acid into the esophagus, leading to symptoms such as heartburn and regurgitation. Hiatus hernia occurs when part of the stomach pushes through the diaphragm into the chest cavity, often contributing to or exacerbating GERD symptoms. Understanding the anatomical disruption in hiatus hernia helps clarify its role in increasing the risk and severity of acid reflux in GERD patients.
Understanding GERD: Definition and Causes
Gastroesophageal reflux disease (GERD) is a chronic condition where stomach acid frequently flows back into the esophagus, causing irritation and symptoms such as heartburn and regurgitation. Hiatus hernia occurs when part of the stomach pushes through the diaphragm into the chest cavity, often contributing to weakened lower esophageal sphincter function and increasing the likelihood of acid reflux. Both conditions disrupt normal esophageal function, but GERD primarily results from dysfunction in the lower esophageal sphincter, while hiatus hernia involves anatomical displacement that exacerbates acid reflux symptoms.
What is a Hiatus Hernia? Types and Risk Factors
A hiatus hernia occurs when part of the stomach pushes through the diaphragm into the chest cavity, commonly classified into sliding and paraesophageal types. Sliding hiatus hernia, the most common form, involves the stomach and esophageal junction moving above the diaphragm, while paraesophageal hernia occurs when part of the stomach herniates alongside the esophagus without displacement of the junction. Risk factors include obesity, aging, pregnancy, smoking, and increased intra-abdominal pressure from heavy lifting or persistent coughing.
Key Differences Between GERD and Hiatus Hernia
Gastroesophageal reflux disease (GERD) primarily involves the backflow of stomach acid into the esophagus, causing symptoms like heartburn and regurgitation due to malfunctioning lower esophageal sphincter. Hiatus hernia occurs when a portion of the stomach protrudes through the diaphragm into the chest cavity, often leading to GERD but can also be asymptomatic. Unlike GERD, hiatus hernia is an anatomical abnormality diagnosed through imaging like endoscopy or barium swallow, whereas GERD diagnosis relies largely on symptomatic assessment and pH monitoring.
Common Symptoms: GERD vs Hiatus Hernia
Gastroesophageal reflux disease (GERD) commonly presents with symptoms such as heartburn, regurgitation, and chest discomfort due to the backflow of stomach acid into the esophagus. Hiatus hernia symptoms often include similar acid reflux signs but can also cause upper abdominal pain, difficulty swallowing, and sometimes bleeding due to the stomach pushing through the diaphragm. Key symptom differentiation lies in GERD's persistent acid-related irritation, while hiatus hernia frequently causes mechanical obstruction and reflux associated with the anatomical defect.
Diagnostic Approaches for GERD and Hiatus Hernia
Diagnostic approaches for Gastroesophageal Reflux Disease (GERD) primarily include upper endoscopy, esophageal pH monitoring, and esophageal manometry to assess acid exposure and esophageal motility. Hiatus hernia diagnosis is commonly achieved through barium swallow radiography and upper endoscopy, which visualize the anatomical displacement of the stomach through the diaphragmatic hiatus. Both conditions may require combined diagnostic methods to differentiate GERD symptoms from anatomical abnormalities identified in hiatus hernia.
Relationship Between GERD and Hiatus Hernia
Hiatus hernia significantly increases the risk of developing gastroesophageal reflux disease (GERD) by weakening the lower esophageal sphincter (LES) and allowing stomach acid to reflux into the esophagus. Studies show that over 60% of patients with GERD have a coexisting hiatus hernia, which exacerbates symptoms such as heartburn and regurgitation. Effective management of GERD often involves addressing the anatomical disruption caused by the hiatus hernia to reduce acid reflux and esophageal irritation.
Treatment Options: Comparing Management Strategies
Gastroesophageal reflux disease (GERD) treatment primarily includes lifestyle modifications, proton pump inhibitors (PPIs), and H2 receptor antagonists to reduce acid production and manage symptoms. Hiatus hernia management varies depending on severity but often involves dietary adjustments, PPIs, and in severe cases, surgical repair such as laparoscopic Nissen fundoplication. Both conditions may benefit from weight loss and avoiding trigger foods, but hiatus hernia might necessitate surgery more frequently due to anatomical defects contributing to reflux.
Lifestyle Changes for Symptom Relief
Lifestyle changes for managing Gastroesophageal Reflux Disease (GERD) emphasize elevating the head of the bed, avoiding large meals before bedtime, and reducing intake of trigger foods like caffeine, alcohol, and spicy dishes to decrease acid reflux. In contrast, lifestyle modifications for hiatus hernia focus on weight management, eating smaller and more frequent meals, and avoiding heavy lifting or straining to prevent hernia protrusion and reduce discomfort. Both conditions benefit from smoking cessation and maintaining an upright posture after eating to aid in symptom relief and improve overall digestive health.
When to Seek Medical Attention
Persistent heartburn and difficulty swallowing are key indicators that medical evaluation is needed for Gastroesophageal reflux disease (GERD) or a hiatus hernia. Immediate medical attention is critical if symptoms include severe chest pain, vomiting blood, or significant weight loss, as these may signal complications such as esophageal damage or obstruction. Regular monitoring is essential for individuals with chronic symptoms to prevent progression and ensure appropriate treatment adjustments.
Gastroesophageal reflux disease (GERD) Infographic
 libterm.com
libterm.com