Asystole, commonly known as flatline, is a critical medical condition characterized by the complete absence of electrical activity in the heart, resulting in no cardiac output and cardiac arrest. Immediate recognition and prompt intervention using advanced cardiac life support protocols are essential for survival. Discover more about the causes, symptoms, and emergency treatments to protect your health in this detailed article.
Table of Comparison
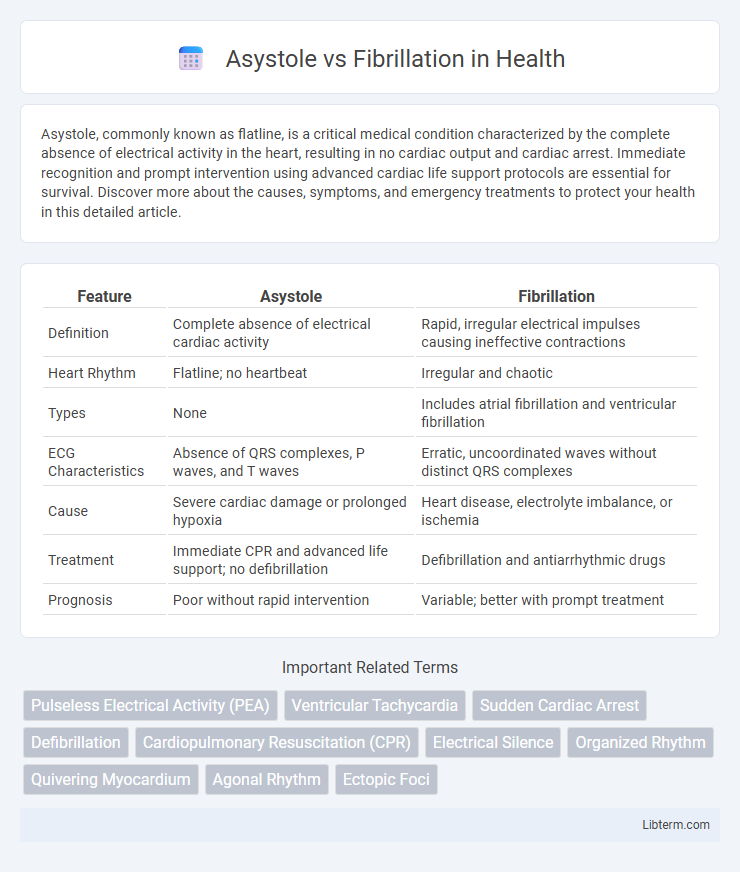
| Feature | Asystole | Fibrillation |
|---|---|---|
| Definition | Complete absence of electrical cardiac activity | Rapid, irregular electrical impulses causing ineffective contractions |
| Heart Rhythm | Flatline; no heartbeat | Irregular and chaotic |
| Types | None | Includes atrial fibrillation and ventricular fibrillation |
| ECG Characteristics | Absence of QRS complexes, P waves, and T waves | Erratic, uncoordinated waves without distinct QRS complexes |
| Cause | Severe cardiac damage or prolonged hypoxia | Heart disease, electrolyte imbalance, or ischemia |
| Treatment | Immediate CPR and advanced life support; no defibrillation | Defibrillation and antiarrhythmic drugs |
| Prognosis | Poor without rapid intervention | Variable; better with prompt treatment |
Introduction to Cardiac Arrest Rhythms
Asystole and fibrillation represent two distinct cardiac arrest rhythms critical for emergency cardiac care. Asystole is characterized by a complete lack of electrical activity in the heart, resulting in a flatline on the ECG and no pulse, making it a non-shockable rhythm. In contrast, fibrillation, including ventricular fibrillation (VF), involves rapid, erratic electrical impulses causing the heart to quiver ineffectively, producing a chaotic ECG pattern that requires immediate defibrillation to restore a perfusing rhythm.
Defining Asystole: The "Flatline
Asystole, commonly known as the "flatline," represents a complete absence of electrical activity in the heart, resulting in no ventricular contractions and zero cardiac output. Unlike fibrillation, which involves chaotic and ineffective electrical impulses causing irregular heartbeats, asystole shows a straight line on an electrocardiogram with no detectable heart rhythm. This condition signifies cardiac arrest and requires immediate advanced life support interventions for potential resuscitation.
Understanding Fibrillation: Chaotic Heart Activity
Fibrillation is characterized by rapid, irregular, and unsynchronized contractions of cardiac muscle fibers, leading to ineffective heart pumping and compromised blood circulation. Unlike asystole, where the heart shows a complete absence of electrical activity and mechanical contraction, fibrillation presents chaotic electrical impulses that disrupt normal cardiac rhythm. Ventricular fibrillation, a critical type of fibrillation, demands immediate defibrillation to restore organized electrical conduction and prevent sudden cardiac arrest.
Causes and Risk Factors for Asystole
Asystole, characterized by the absence of electrical activity in the heart, often results from prolonged cardiac arrest, severe hypoxia, or advanced myocardial infarction. Unlike fibrillation, which involves erratic electrical activity causing ineffective contractions, asystole is primarily caused by factors such as electrolyte imbalances, drug overdose, or significant trauma leading to cardiac electrical failure. Risk factors for asystole include existing heart disease, respiratory failure, and untreated arrhythmias, which impair the heart's ability to maintain electrical conduction.
Causes and Risk Factors for Fibrillation
Fibrillation, including atrial fibrillation and ventricular fibrillation, is primarily caused by abnormal electrical signals in the heart, often triggered by heart disease, hypertension, or electrolyte imbalances. Risk factors for fibrillation include advanced age, coronary artery disease, heart valve disorders, high blood pressure, and excessive alcohol consumption. Unlike asystole, which is characterized by a complete absence of electrical activity, fibrillation involves rapid, irregular heartbeats that significantly impair cardiac function.
Clinical Presentation: Asystole vs Fibrillation
Asystole presents clinically as unresponsive pulselessness with no detectable electrical activity on the ECG, often indicating the absence of cardiac output. Fibrillation, particularly ventricular fibrillation, manifests as sudden collapse, loss of consciousness, and erratic, rapid ECG waveforms representing chaotic ventricular activity without effective contractions. Both conditions require immediate intervention, but fibrillation may initially retain some cardiac output before progressing to complete cardiac arrest unlike asystole, which shows no signs of electrical conduction or myocardial contractility.
Diagnostic Approaches and ECG Findings
Asystole presents as a flatline on an ECG, indicating complete absence of electrical activity and making immediate confirmation through multiple leads crucial to avoid misdiagnosis. Fibrillation, including atrial or ventricular, exhibits chaotic, irregular waveforms on the ECG, with ventricular fibrillation showing irregular, rapid, and erratic electrical activity while atrial fibrillation displays absent P waves and irregularly irregular QRS complexes. Diagnostic approaches prioritize rapid ECG interpretation, with asystole requiring prompt recognition of absent QRS complexes and fibrillation identified by irregular rhythm patterns to guide resuscitation and treatment decisions effectively.
Emergency Treatment Protocols
Emergency treatment protocols for asystole prioritize immediate CPR and advanced cardiac life support (ACLS) interventions, including administering epinephrine while confirming the absence of reversible causes. In contrast, fibrillation, specifically ventricular fibrillation, requires prompt defibrillation alongside high-quality CPR to restore organized cardiac rhythm. Both conditions demand rapid assessment and continuous monitoring to improve survival outcomes and prevent irreversible cardiac damage.
Prognosis and Survival Rates
Asystole, characterized by the complete absence of electrical activity in the heart, has a significantly poorer prognosis with survival rates often below 5% due to the lack of effective cardiac output and limited response to resuscitation efforts. Fibrillation, including ventricular fibrillation, presents chaotic and uncoordinated electrical activity, but rapid defibrillation can improve survival rates up to 50%, especially with immediate advanced cardiac life support. The difference in survival outcomes emphasizes the critical importance of timely intervention, with fibrillation being more reversible compared to the near-fatal nature of asystole.
Prevention and Long-Term Management
Effective prevention of asystole and fibrillation involves maintaining heart health through regular cardiovascular screenings, management of underlying conditions such as coronary artery disease, and lifestyle modifications like quitting smoking and controlling hypertension. Long-term management includes the use of implantable cardioverter defibrillators (ICDs) for fibrillation to detect and correct arrhythmias promptly, while asystole often requires advanced cardiac life support interventions and addressing reversible causes. Continuous monitoring, adherence to prescribed medications such as beta-blockers or antiarrhythmics, and routine follow-up with cardiologists are critical for reducing recurrence and improving patient outcomes.
Asystole Infographic
 libterm.com
libterm.com