Sarcoidosis and hypersensitivity pneumonitis are inflammatory lung diseases characterized by immune system reactions causing granuloma formation and lung tissue damage. Both conditions present with respiratory symptoms, but sarcoidosis is a systemic disease affecting multiple organs, while hypersensitivity pneumonitis results from inhaled environmental antigens leading to lung inflammation. Discover how to differentiate these conditions and manage your respiratory health by exploring the rest of this article.
Table of Comparison
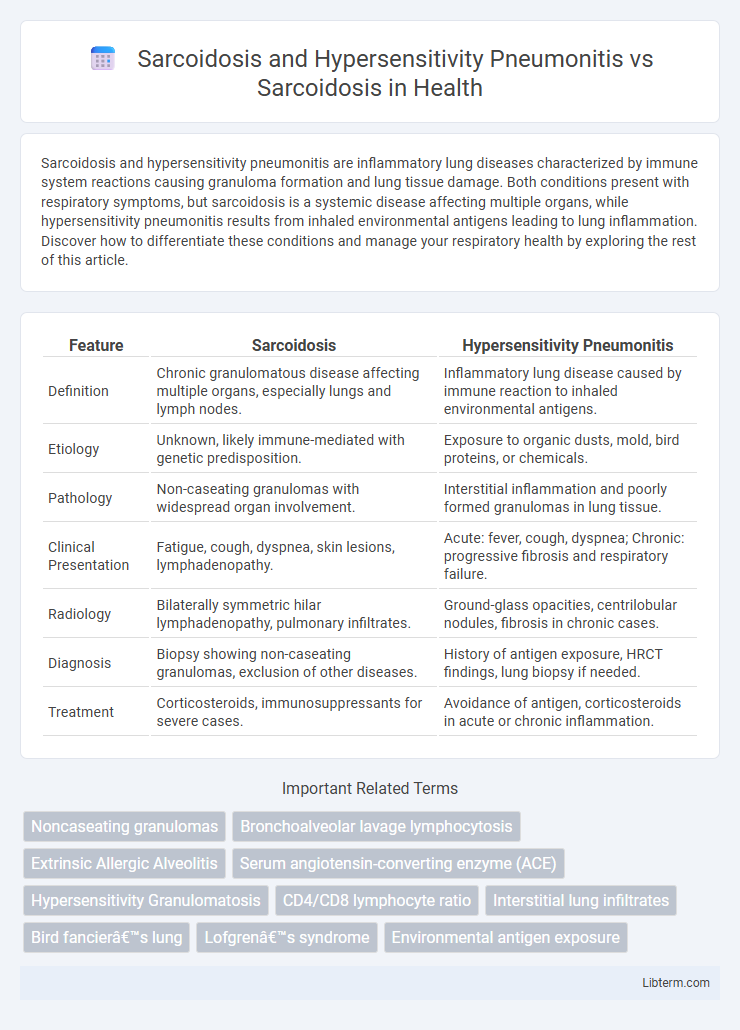
| Feature | Sarcoidosis | Hypersensitivity Pneumonitis |
|---|---|---|
| Definition | Chronic granulomatous disease affecting multiple organs, especially lungs and lymph nodes. | Inflammatory lung disease caused by immune reaction to inhaled environmental antigens. |
| Etiology | Unknown, likely immune-mediated with genetic predisposition. | Exposure to organic dusts, mold, bird proteins, or chemicals. |
| Pathology | Non-caseating granulomas with widespread organ involvement. | Interstitial inflammation and poorly formed granulomas in lung tissue. |
| Clinical Presentation | Fatigue, cough, dyspnea, skin lesions, lymphadenopathy. | Acute: fever, cough, dyspnea; Chronic: progressive fibrosis and respiratory failure. |
| Radiology | Bilaterally symmetric hilar lymphadenopathy, pulmonary infiltrates. | Ground-glass opacities, centrilobular nodules, fibrosis in chronic cases. |
| Diagnosis | Biopsy showing non-caseating granulomas, exclusion of other diseases. | History of antigen exposure, HRCT findings, lung biopsy if needed. |
| Treatment | Corticosteroids, immunosuppressants for severe cases. | Avoidance of antigen, corticosteroids in acute or chronic inflammation. |
Overview of Sarcoidosis
Sarcoidosis is a multisystem inflammatory disease characterized by the formation of noncaseating granulomas, primarily affecting the lungs and lymphatic system. Unlike Hypersensitivity Pneumonitis, which results from inhalation of environmental antigens triggering an immune response, sarcoidosis has an unclear etiology often linked to genetic predisposition and immune system dysregulation. Diagnosis relies on clinical evaluation, imaging showing bilateral hilar lymphadenopathy, and histological confirmation of granulomas without evidence of infection or foreign material.
Overview of Hypersensitivity Pneumonitis
Hypersensitivity pneumonitis (HP) is an immune-mediated lung disease characterized by inflammation of the alveoli and interstitium due to inhaled environmental antigens, such as mold, bird proteins, or chemical dust. Unlike sarcoidosis, which involves non-caseating granulomas of unknown etiology affecting multiple organs, HP specifically results from repeated antigen exposure causing a hypersensitivity reaction predominantly in the lungs. Accurate diagnosis of HP involves identifying antigen exposure history, radiographic patterns like ground-glass opacities and fibrosis, and lung biopsy showing lymphocytic infiltration and poorly formed granulomas.
Epidemiology: Sarcoidosis vs Hypersensitivity Pneumonitis
Sarcoidosis predominantly affects adults between 20 and 40 years of age, with a higher incidence in African Americans and Northern Europeans, showing a prevalence of approximately 10 to 20 cases per 100,000 individuals worldwide. Hypersensitivity pneumonitis (HP) occurs across all adult age groups but is more common in individuals exposed to occupational or environmental antigens, with prevalence rates varying widely from 0.9 to 2.7 cases per 100,000 in general populations and higher in specific high-exposure cohorts. Unlike sarcoidosis, which has a consistent demographic pattern, HP incidence is closely linked to geographic and occupational factors, reflecting exposure variability and influencing epidemiological distribution.
Risk Factors and Triggers
Sarcoidosis primarily affects adults aged 20-40 and is influenced by genetic predisposition, with higher prevalence in African Americans and Northern Europeans. Hypersensitivity pneumonitis arises from repeated inhalation of environmental antigens such as mold, bird proteins, or agricultural dust, triggering immune-mediated lung inflammation. Unlike sarcoidosis, hypersensitivity pneumonitis risk is strongly linked to occupational or hobby-related exposures, whereas sarcoidosis risk factors include ethnicity, family history, and certain infections.
Pathophysiology: Comparing Mechanisms
Sarcoidosis involves noncaseating granuloma formation driven by an exaggerated immune response to unidentified antigens, primarily activating CD4+ T-helper cells and macrophages in affected tissues. Hypersensitivity Pneumonitis results from repeated inhalation of environmental antigens, triggering type III and IV hypersensitivity reactions with immune complex deposition and granulomatous inflammation in alveoli. While both diseases feature granuloma formation, sarcoidosis shows systemic immune dysregulation, whereas hypersensitivity pneumonitis is characterized by antigen-specific immune responses leading to lung-restricted pathology.
Clinical Symptoms and Presentation
Sarcoidosis typically presents with bilateral hilar lymphadenopathy, pulmonary infiltrates, and symptoms like persistent dry cough, fatigue, and erythema nodosum, contrasting with Hypersensitivity Pneumonitis (HP), which often manifests as acute episodes of fever, chills, cough, and dyspnea following antigen exposure. Chronic HP may mimic sarcoidosis with progressive dyspnea and fibrosis but is distinguished by a history of exposure to organic dusts or molds and presence of granulomatous inflammation in lung biopsy. Both conditions share granulomatous inflammation but differ in clinical triggers, symptom onset, and immunologic response patterns, crucial for accurate diagnosis and management.
Diagnostic Criteria: Sarcoidosis and HP
Sarcoidosis diagnosis relies on clinical presentation, noncaseating granulomas on biopsy, and exclusion of other granulomatous diseases, supported by imaging such as bilateral hilar lymphadenopathy on chest X-ray or CT. Hypersensitivity pneumonitis diagnosis integrates exposure history to relevant antigens, radiographic findings demonstrating ground-glass opacities or mosaic attenuation, positive specific IgG antibodies, and lung biopsy showing cellular interstitial infiltrates with poorly formed granulomas. Differentiating factors include sarcoidosis's predilection for well-formed granulomas and lymphatic distribution versus HP's diffuse inflammation with centrilobular emphasis and history of antigen exposure.
Radiological and Histological Differences
Sarcoidosis typically presents with bilateral hilar lymphadenopathy and perilymphatic nodules predominantly in the upper lung zones on radiological imaging, while Hypersensitivity Pneumonitis (HP) often shows centrilobular ground-glass nodules and mosaic attenuation due to air trapping. Histologically, sarcoidosis is characterized by non-caseating granulomas with tightly clustered epithelioid cells and minimal surrounding inflammation, whereas HP demonstrates poorly formed granulomas accompanied by a lymphocytic interstitial infiltrate and bronchiolitis. These distinct radiologic and histopathologic features are crucial for differential diagnosis and targeted management of each granulomatous lung disease.
Treatment and Management Approaches
Treatment of sarcoidosis primarily involves corticosteroids to reduce granulomatous inflammation, with immunosuppressive agents like methotrexate or azathioprine used for refractory cases. Hypersensitivity pneumonitis management centers on antigen avoidance and corticosteroid therapy to control inflammation, with chronic cases sometimes requiring immunosuppressive treatment. Both conditions demand regular monitoring of pulmonary function and symptom assessment to tailor therapy and prevent progression.
Prognosis and Long-Term Outcomes
Sarcoidosis prognosis varies with the extent of organ involvement, with many patients experiencing spontaneous remission within 3-5 years, while 10-20% progress to chronic disease leading to pulmonary fibrosis or organ failure. Hypersensitivity pneumonitis (HP) prognosis depends heavily on early antigen avoidance; chronic HP often results in irreversible lung fibrosis and worse long-term outcomes compared to sarcoidosis. Long-term management in sarcoidosis emphasizes monitoring for pulmonary and extrapulmonary complications, whereas in HP, prognosis improves significantly with environmental control, although fibrotic HP carries a poorer prognosis similar to idiopathic pulmonary fibrosis.
Sarcoidosis and Hypersensitivity Pneumonitis Infographic
 libterm.com
libterm.com