Asystole is a critical cardiac condition characterized by the absence of electrical activity in the heart, leading to a flatline on an ECG and no detectable heartbeat. Immediate medical intervention is necessary to restore cardiac function and prevent irreversible organ damage. Explore the rest of the article to understand causes, treatment options, and survival strategies for asystole.
Table of Comparison
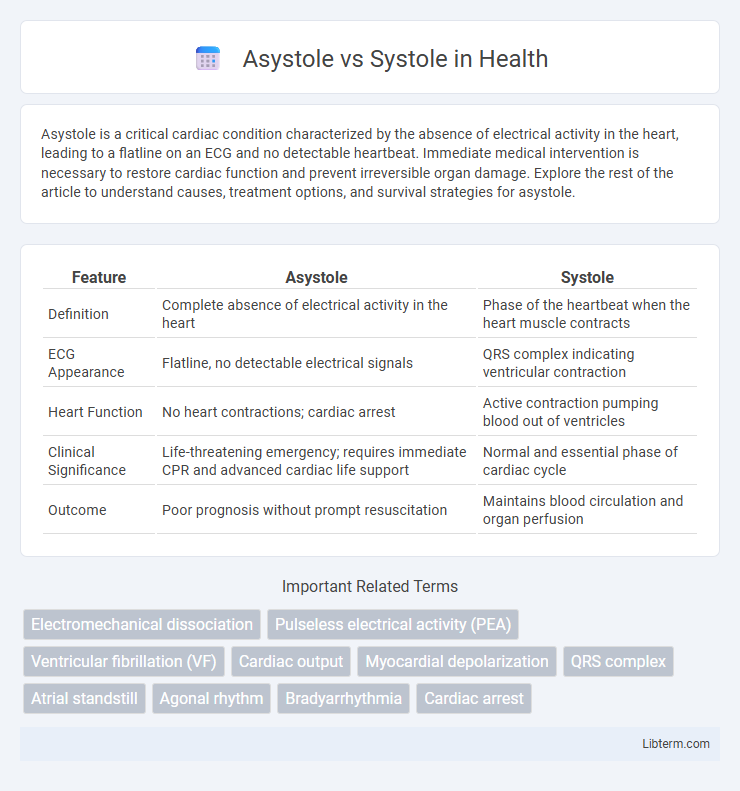
| Feature | Asystole | Systole |
|---|---|---|
| Definition | Complete absence of electrical activity in the heart | Phase of the heartbeat when the heart muscle contracts |
| ECG Appearance | Flatline, no detectable electrical signals | QRS complex indicating ventricular contraction |
| Heart Function | No heart contractions; cardiac arrest | Active contraction pumping blood out of ventricles |
| Clinical Significance | Life-threatening emergency; requires immediate CPR and advanced cardiac life support | Normal and essential phase of cardiac cycle |
| Outcome | Poor prognosis without prompt resuscitation | Maintains blood circulation and organ perfusion |
Understanding Asystole: Definition and Causes
Asystole is a critical cardiac condition characterized by the complete absence of electrical activity and ventricular contractions, resulting in no heartbeat and no blood flow. It contrasts with systole, the phase in the cardiac cycle where the heart muscles contract to pump blood out of the chambers, maintaining circulation. Common causes of asystole include severe cardiac arrest, electrolyte imbalances, hypoxia, and drug overdose, which disrupt the heart's electrical system and prevent effective cardiac output.
Systole Explained: The Heart’s Contractile Phase
Systole is the phase of the cardiac cycle during which the heart's ventricles contract, pumping oxygenated blood into the aorta and pulmonary artery. This contractile phase increases ventricular pressure, closes the atrioventricular valves, and opens the semilunar valves to ensure efficient blood flow. Asystole, in contrast, is a state of cardiac arrest characterized by a complete absence of electrical activity and ventricular contraction, resulting in no blood flow.
Electrical Activity Differences: Asystole vs Systole
Asystole is characterized by a complete absence of electrical activity in the heart, resulting in no ventricular contractions and a flatline ECG. In contrast, systole refers to the phase of the cardiac cycle where electrical impulses trigger ventricular contraction, generating a distinct QRS complex on the ECG. The key electrical difference lies in asystole's total electrical silence versus systole's coordinated depolarization and contraction signals.
Clinical Manifestations and Symptoms
Asystole presents with complete absence of cardiac electrical activity, leading to no palpable pulse, loss of consciousness, and apnea, signaling cardiac arrest that requires immediate resuscitation. Systole, as the phase of ventricular contraction, manifests clinically with a palpable pulse and systolic blood pressure, essential for effective tissue perfusion and patient hemodynamics. Recognizing the absence of mechanical and electrical activity in asystole versus the normal contraction in systole is critical for accurate diagnosis and timely management in emergency cardiac care.
ECG Findings: Asystole vs Systole
Asystole on an ECG presents as a flatline with no discernible P waves, QRS complexes, or T waves, indicating complete absence of electrical cardiac activity. In contrast, systole is the phase of the cardiac cycle where the ventricles contract, typically represented on an ECG by the QRS complex, reflecting ventricular depolarization. The key difference lies in the presence of electrical signals during systole, whereas asystole shows no electrical activity, signifying cardiac arrest.
Underlying Pathophysiology
Asystole represents a complete cessation of electrical activity in the heart, leading to the absence of myocardial depolarization and cardiac contractions, typically caused by severe ischemia, electrolyte imbalances, or profound hypoxia. Systole, in contrast, refers to the phase of the cardiac cycle where ventricular contraction occurs due to coordinated depolarization and calcium-induced myocardial fiber shortening, enabling blood ejection into the systemic and pulmonary circulations. The underlying pathophysiology of asystole involves failure of the sinoatrial node or conduction system, whereas systole depends on intact cardiac conduction pathways and sufficient myocardial oxygen supply to generate effective contractile force.
Common Triggers and Risk Factors
Asystole, characterized by a complete absence of electrical activity in the heart, is commonly triggered by severe cardiac arrest, electrolyte imbalances, or prolonged hypoxia, whereas systole refers to the phase of the cardiac cycle when the heart muscle contracts to pump blood. Risk factors for asystole include advanced heart disease, severe electrolyte disturbances, and respiratory failure, while systolic dysfunction is often associated with high blood pressure, myocardial infarction, and cardiomyopathy. Understanding these triggers and risk factors is critical for timely diagnosis and effective management of cardiac events.
Emergency Response Protocols
Asystole, characterized by a complete absence of electrical activity in the heart, requires immediate initiation of cardiopulmonary resuscitation (CPR) and administration of epinephrine according to advanced cardiac life support (ACLS) protocols, as defibrillation is ineffective. In contrast, systole refers to the contraction phase of the cardiac cycle where the heart pumps blood; emergency response focuses on maintaining adequate blood pressure and cardiac output during systolic failure, often using inotropic agents. Rapid identification and differentiation between asystole and systolic dysfunction are critical for implementing targeted treatment strategies and improving patient survival outcomes.
Treatment Approaches for Asystole and Systole
Asystole, characterized by the absence of electrical activity and no cardiac output, requires immediate initiation of cardiopulmonary resuscitation (CPR) and administration of epinephrine to enhance myocardial and cerebral perfusion. Systole, the phase of cardiac contraction, is not treated directly, but disorders affecting systolic function such as heart failure are managed using medications like beta-blockers, ACE inhibitors, and diuretics to improve cardiac output. Advanced cardiac life support protocols emphasize rapid recognition and intervention in asystole to increase chances of return of spontaneous circulation, while systolic dysfunction treatments focus on long-term management and symptom relief.
Prognosis and Patient Outcomes
Asystole, characterized by the complete absence of electrical activity in the heart, generally has a poor prognosis with survival rates below 5% without immediate advanced cardiac life support interventions. In contrast, systole refers to the phase of cardiac contraction responsible for pumping blood, and preserved systolic function is associated with better patient outcomes and lower mortality in various cardiac conditions. Effective management of systolic heart failure improves prognosis significantly, whereas asystole requires urgent resuscitation efforts to prevent irreversible organ damage.
Asystole Infographic
 libterm.com
libterm.com