Dacryocystitis is an infection of the tear sac that causes redness, swelling, and pain near the inner corner of the eye, while orbital cellulitis is a serious infection of the tissues surrounding the eye, potentially leading to vision loss if untreated. Both conditions require prompt medical attention to prevent complications and preserve eye health. Explore this article to learn how to recognize symptoms and understand effective treatment options for your eye's safety.
Table of Comparison
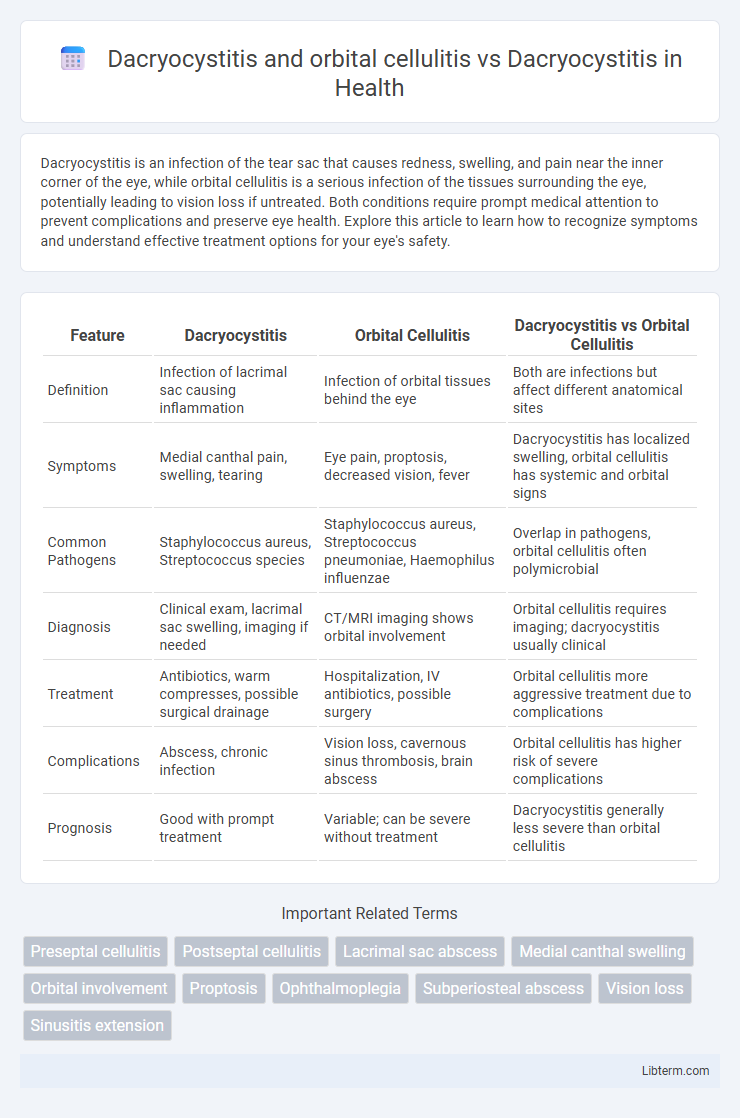
| Feature | Dacryocystitis | Orbital Cellulitis | Dacryocystitis vs Orbital Cellulitis |
|---|---|---|---|
| Definition | Infection of lacrimal sac causing inflammation | Infection of orbital tissues behind the eye | Both are infections but affect different anatomical sites |
| Symptoms | Medial canthal pain, swelling, tearing | Eye pain, proptosis, decreased vision, fever | Dacryocystitis has localized swelling, orbital cellulitis has systemic and orbital signs |
| Common Pathogens | Staphylococcus aureus, Streptococcus species | Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae | Overlap in pathogens, orbital cellulitis often polymicrobial |
| Diagnosis | Clinical exam, lacrimal sac swelling, imaging if needed | CT/MRI imaging shows orbital involvement | Orbital cellulitis requires imaging; dacryocystitis usually clinical |
| Treatment | Antibiotics, warm compresses, possible surgical drainage | Hospitalization, IV antibiotics, possible surgery | Orbital cellulitis more aggressive treatment due to complications |
| Complications | Abscess, chronic infection | Vision loss, cavernous sinus thrombosis, brain abscess | Orbital cellulitis has higher risk of severe complications |
| Prognosis | Good with prompt treatment | Variable; can be severe without treatment | Dacryocystitis generally less severe than orbital cellulitis |
Introduction to Dacryocystitis and Orbital Cellulitis
Dacryocystitis is an infection of the lacrimal sac, characterized by pain, swelling, and redness near the inner corner of the eye. Orbital cellulitis involves an infection of the tissues surrounding the eye, presenting with symptoms such as severe eyelid edema, proptosis, and impaired ocular motility. Early differentiation between dacryocystitis and orbital cellulitis is critical due to the latter's potential for rapid progression to vision-threatening complications.
Understanding Dacryocystitis: Causes and Risk Factors
Dacryocystitis is an infection of the lacrimal sac, primarily caused by nasolacrimal duct obstruction leading to bacterial stasis and proliferation, commonly involving Staphylococcus aureus and Streptococcus species. Risk factors include chronic nasolacrimal duct obstruction, trauma, eyelid abnormalities, and systemic conditions such as diabetes mellitus that impair immune response. Differentiating dacryocystitis from orbital cellulitis is critical, as orbital cellulitis involves infection posterior to the orbital septum with potential for rapid spread and vision-threatening complications, whereas dacryocystitis is localized to the lacrimal sac region.
Orbital Cellulitis: Pathogenesis and Etiology
Orbital cellulitis is an acute infection of the orbital tissues posterior to the orbital septum, primarily caused by bacterial spread from adjacent structures such as the ethmoid sinuses. The pathogenesis involves rapid bacterial invasion leading to inflammation, edema, and potential abscess formation, posing risks of vision loss and intracranial complications. Common etiological agents include Streptococcus species, Staphylococcus aureus, and Haemophilus influenzae, with sinusitis being the most frequent predisposing factor distinguishing it from isolated dacryocystitis, which is confined to the lacrimal sac infection.
Clinical Presentation: Dacryocystitis vs. Orbital Cellulitis
Dacryocystitis presents with localized pain, swelling, and redness at the medial canthus, often accompanied by tearing and purulent discharge from the lacrimal punctum. Orbital cellulitis manifests with more severe symptoms including proptosis, restricted extraocular movements, ophthalmoplegia, and potential vision impairment, indicating deeper orbital involvement. Differentiating clinical features such as absence of proptosis and confined swelling help distinguish dacryocystitis from the more extensive orbital cellulitis.
Diagnostic Approaches: Imaging and Laboratory Tests
Dacryocystitis diagnosis relies on clinical examination supported by imaging techniques such as dacryocystography or ultrasound to visualize the lacrimal sac and confirm obstruction or abscess formation, while orbital cellulitis requires urgent orbital CT or MRI to assess the extent of orbital involvement and rule out complications like subperiosteal abscess. Laboratory tests including complete blood count and inflammatory markers (CRP, ESR) assist in identifying infection severity in both conditions, with blood cultures recommended in orbital cellulitis to detect systemic spread. Differentiating between these infections hinges on imaging findings and clinical presentation, guiding appropriate medical or surgical intervention.
Key Differences in Symptoms and Signs
Dacryocystitis primarily presents with localized pain, swelling, and redness over the lacrimal sac near the inner corner of the eye, often accompanied by purulent discharge and tearing. Orbital cellulitis, in contrast, exhibits more severe systemic symptoms including fever, proptosis, restricted eye movement, and decreased visual acuity, indicating infection spread to the orbit. Unlike isolated dacryocystitis, orbital cellulitis demands urgent intervention due to the risk of vision loss and intracranial complications.
Complications: Isolated Dacryocystitis and Spread to Orbit
Dacryocystitis, an infection of the lacrimal sac, primarily causes localized pain, swelling, and erythema near the medial canthus, with complications typically limited to abscess formation or chronic lacrimal duct obstruction. When infection spreads beyond the lacrimal sac, it can extend into the orbit, leading to orbital cellulitis characterized by proptosis, ophthalmoplegia, decreased visual acuity, and potential risk of vision loss or intracranial complications. Early differentiation between isolated dacryocystitis and orbital cellulitis is critical, as orbital involvement requires aggressive intravenous antibiotics and possible surgical intervention to prevent permanent ocular damage.
Treatment Options: Medical and Surgical Management
Treatment options for dacryocystitis primarily include systemic antibiotics targeting common pathogens like Staphylococcus aureus and Streptococcus species, with warm compresses aiding symptom relief; surgical intervention such as dacryocystorhinostomy (DCR) is considered for chronic or recurrent cases to restore lacrimal drainage. Orbital cellulitis requires aggressive intravenous antibiotic therapy covering polymicrobial infections, often including broad-spectrum agents targeting Staphylococcus aureus, Streptococci, and anaerobes, combined with close monitoring for abscess formation necessitating surgical drainage. Early differentiation between dacryocystitis and orbital cellulitis is critical for appropriate management, as orbital cellulitis poses a higher risk of complications and typically demands more urgent, intensive medical and sometimes surgical treatment.
Prognosis and Outcomes: Comparative Analysis
Dacryocystitis typically presents with localized inflammation of the lacrimal sac and has a favorable prognosis when treated promptly with antibiotics or surgical intervention, with most patients achieving full recovery without complications. In contrast, orbital cellulitis, a more severe infection involving the orbital tissues, carries a risk of serious complications such as vision loss, abscess formation, and intracranial spread, resulting in a less favorable prognosis and often requiring aggressive intravenous antibiotics and possible surgical drainage. Early diagnosis and appropriate management significantly improve outcomes in both conditions, but the potential for morbidity is markedly higher in orbital cellulitis compared to isolated dacryocystitis.
Prevention and Early Detection Strategies
Dacryocystitis prevention centers on maintaining proper eyelid hygiene and prompt treatment of nasolacrimal duct obstruction to reduce infection risk. Early detection involves recognizing symptoms such as redness, swelling near the lacrimal sac, and tearing, which differentiates it from orbital cellulitis that presents with pain, fever, and impaired eye movement. Regular ophthalmologic evaluations and immediate antibiotic therapy can prevent complications like orbital cellulitis, which requires urgent intervention to avoid vision loss.
Dacryocystitis and orbital cellulitis Infographic
 libterm.com
libterm.com