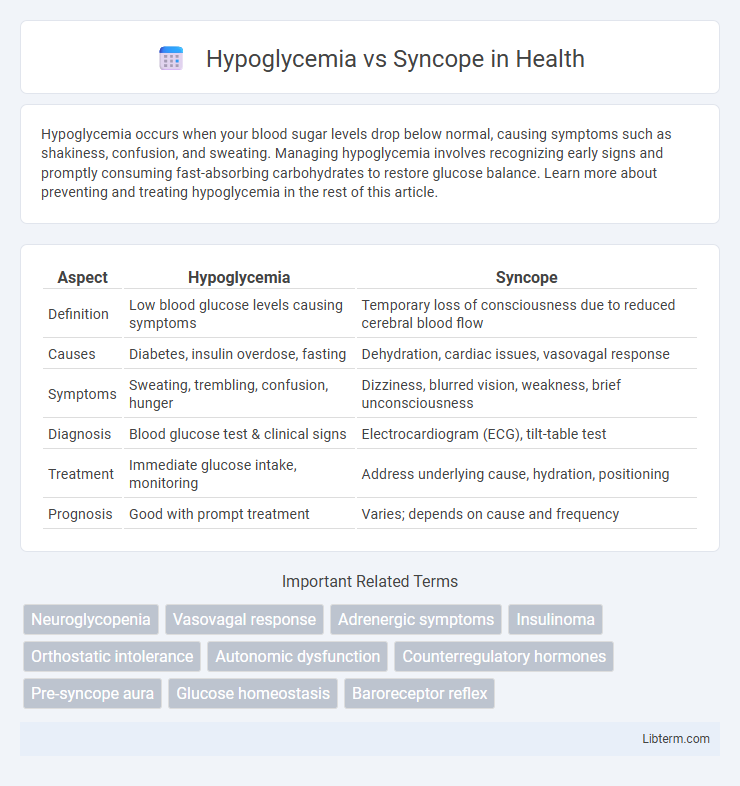
Hypoglycemia occurs when your blood sugar levels drop below normal, causing symptoms such as shakiness, confusion, and sweating. Managing hypoglycemia involves recognizing early signs and promptly consuming fast-absorbing carbohydrates to restore glucose balance. Learn more about preventing and treating hypoglycemia in the rest of this article.
Table of Comparison
| Aspect | Hypoglycemia | Syncope |
|---|---|---|
| Definition | Low blood glucose levels causing symptoms | Temporary loss of consciousness due to reduced cerebral blood flow |
| Causes | Diabetes, insulin overdose, fasting | Dehydration, cardiac issues, vasovagal response |
| Symptoms | Sweating, trembling, confusion, hunger | Dizziness, blurred vision, weakness, brief unconsciousness |
| Diagnosis | Blood glucose test & clinical signs | Electrocardiogram (ECG), tilt-table test |
| Treatment | Immediate glucose intake, monitoring | Address underlying cause, hydration, positioning |
| Prognosis | Good with prompt treatment | Varies; depends on cause and frequency |
Understanding Hypoglycemia: Definition and Causes
Hypoglycemia is a medical condition characterized by abnormally low blood glucose levels, typically below 70 mg/dL, which can impair brain function and trigger symptoms such as dizziness, sweating, and confusion. Common causes include excessive insulin administration in diabetic patients, prolonged fasting, certain medications, and endocrine disorders like adrenal insufficiency. Understanding hypoglycemia is crucial for differentiating it from syncope, as both conditions may present with similar manifestations but require distinct diagnostic approaches and treatments.
What is Syncope? Types and Triggers
Syncope is a temporary loss of consciousness caused by a sudden drop in blood flow to the brain, often resulting from cardiovascular or neurological factors. Types of syncope include vasovagal (triggered by stress or pain), situational (caused by specific actions like coughing or urination), and cardiac syncope (due to heart conditions such as arrhythmias). Common triggers involve dehydration, prolonged standing, emotional distress, and underlying heart disease, distinguishing it from hypoglycemia, which is primarily linked to low blood sugar levels.
Pathophysiology: How Hypoglycemia and Syncope Differ
Hypoglycemia results from abnormally low blood glucose levels causing neuroglycopenia, which impairs cerebral function and triggers symptoms like sweating, confusion, and loss of consciousness. Syncope primarily arises from transient global cerebral hypoperfusion due to cardiovascular abnormalities, leading to sudden loss of consciousness without the metabolic disturbances seen in hypoglycemia. The pathophysiological distinction lies in hypoglycemia's metabolic insufficiency versus syncope's hemodynamic insufficiency affecting brain oxygen delivery.
Key Symptoms: Differentiating Hypoglycemia and Syncope
Hypoglycemia primarily presents with symptoms such as sweating, tremors, confusion, and hunger due to low blood glucose levels, while syncope is characterized by a sudden loss of consciousness and muscle tone typically caused by transient cerebral hypoperfusion. Key distinguishing symptoms include the presence of neuroglycopenic signs like dizziness, weakness, and blurred vision in hypoglycemia, contrasted with pallor, brief convulsive movements, and rapid recovery in syncope. Accurate differentiation relies on monitoring blood glucose levels during episodes and assessing prodromal symptoms alongside clinical history.
Risk Factors for Hypoglycemia vs Syncope
Risk factors for hypoglycemia include diabetes management with insulin or oral hypoglycemics, prolonged fasting, excessive alcohol consumption, and certain critical illnesses like liver or kidney disease. Syncope is commonly associated with cardiovascular conditions such as arrhythmias or aortic stenosis, dehydration, autonomic dysfunction, and vasovagal triggers like emotional stress or pain. Both conditions share overlapping triggers like medication effects and inadequate nutrition, but their underlying risk profiles differ significantly based on metabolic versus circulatory causes.
Diagnostic Approaches: Identifying the Root Cause
Differentiating hypoglycemia from syncope relies heavily on targeted diagnostic approaches such as blood glucose measurement during symptomatic episodes for identifying neuroglycopenia. Electrocardiograms and tilt-table tests are crucial in syncope evaluation to detect cardiac arrhythmias or vasovagal responses. Comprehensive patient history combined with laboratory assessments including plasma glucose, insulin levels, and cardiac monitoring ensures accurate identification of the underlying cause.
Acute Management Strategies for Each Condition
Acute management of hypoglycemia involves rapid administration of glucose, either orally if the patient is conscious or intravenously via dextrose solution if unconscious, alongside continuous monitoring of blood glucose levels to prevent recurrence. In contrast, syncope requires immediate assessment of airway, breathing, and circulation, with prompt positioning of the patient in a supine or Trendelenburg position to restore cerebral perfusion, coupled with identification and treatment of underlying causes such as cardiac arrhythmias or orthostatic hypotension. Both conditions necessitate tailored interventions targeting the root physiological disturbances to ensure effective stabilization and recovery.
Long-Term Prevention and Patient Education
Effective long-term prevention of hypoglycemia involves consistent blood glucose monitoring, tailored medication management, and nutritional counseling to maintain stable glucose levels, particularly for diabetic patients using insulin or sulfonylureas. Syncope prevention requires identifying and managing underlying causes such as cardiovascular or neurological disorders, combined with patient education on recognizing prodromal symptoms and adopting lifestyle modifications like adequate hydration and avoiding prolonged standing. Comprehensive patient education emphasizing symptom awareness, timely intervention, and adherence to treatment protocols is crucial in reducing recurrence rates and improving overall quality of life for individuals prone to hypoglycemic episodes or syncope.
Serious Complications: Why Accurate Diagnosis Matters
Hypoglycemia can cause seizures, brain damage, and even death if untreated, while syncope may result from cardiac arrhythmias leading to sudden cardiac arrest. Accurate diagnosis is crucial to prevent these serious complications by guiding appropriate treatment, such as glucose administration for hypoglycemia or cardiac monitoring and intervention for syncope. Misdiagnosis increases risks of recurrent episodes and worsens prognosis, emphasizing the need for precise clinical evaluation and timely diagnostic tests.
When to Seek Medical Attention: Red Flags
Seek immediate medical attention for hypoglycemia if symptoms include persistent confusion, seizures, or loss of consciousness, as these indicate severe blood sugar drops requiring urgent intervention. Syncope warrants emergency evaluation when accompanied by chest pain, palpitations, or neurological deficits, suggesting potential cardiac or cerebrovascular causes. Both conditions demand prompt assessment to prevent life-threatening complications and ensure appropriate treatment.
Hypoglycemia Infographic
 libterm.com
libterm.com