Cyanosis is a condition characterized by a bluish discoloration of the skin and mucous membranes due to inadequate oxygen levels in the blood. It often signals underlying issues such as respiratory or cardiovascular problems that require prompt medical attention. Discover more about the causes, symptoms, and treatments of cyanosis in the rest of this article.
Table of Comparison
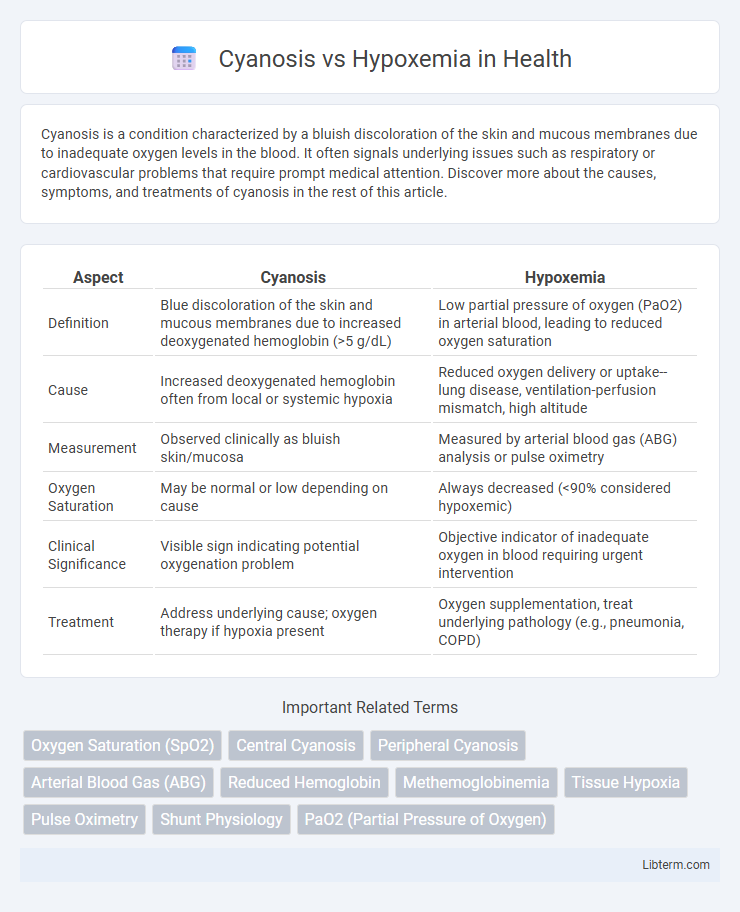
| Aspect | Cyanosis | Hypoxemia |
|---|---|---|
| Definition | Blue discoloration of the skin and mucous membranes due to increased deoxygenated hemoglobin (>5 g/dL) | Low partial pressure of oxygen (PaO2) in arterial blood, leading to reduced oxygen saturation |
| Cause | Increased deoxygenated hemoglobin often from local or systemic hypoxia | Reduced oxygen delivery or uptake--lung disease, ventilation-perfusion mismatch, high altitude |
| Measurement | Observed clinically as bluish skin/mucosa | Measured by arterial blood gas (ABG) analysis or pulse oximetry |
| Oxygen Saturation | May be normal or low depending on cause | Always decreased (<90% considered hypoxemic) |
| Clinical Significance | Visible sign indicating potential oxygenation problem | Objective indicator of inadequate oxygen in blood requiring urgent intervention |
| Treatment | Address underlying cause; oxygen therapy if hypoxia present | Oxygen supplementation, treat underlying pathology (e.g., pneumonia, COPD) |
Understanding Cyanosis: Definition and Causes
Cyanosis is a clinical condition characterized by a bluish or purplish discoloration of the skin and mucous membranes due to insufficient oxygenation of hemoglobin in the blood. It arises when deoxygenated hemoglobin exceeds 5 g/dL in capillary blood, commonly caused by respiratory diseases, congenital heart defects, or circulatory problems impairing oxygen delivery. Hypoxemia, on the other hand, refers specifically to low oxygen levels in arterial blood, which may or may not result in visible cyanosis depending on factors like hemoglobin concentration and tissue perfusion.
What is Hypoxemia? Key Concepts Explained
Hypoxemia is a medical condition characterized by abnormally low levels of oxygen in the arterial blood, typically measured by a partial pressure of oxygen (PaO2) below 80 mmHg or oxygen saturation under 90%. It results from impaired gas exchange in the lungs, ventilation-perfusion mismatch, or reduced oxygen-carrying capacity of the blood. Unlike cyanosis, which is a visible bluish discoloration of the skin caused by increased deoxygenated hemoglobin, hypoxemia is a physiological state that may or may not manifest with cyanosis depending on its severity and duration.
Cyanosis vs Hypoxemia: Major Differences
Cyanosis is a clinical sign characterized by a bluish discoloration of the skin and mucous membranes, typically indicating inadequate oxygenation of hemoglobin in the blood. Hypoxemia refers to a lower than normal partial pressure of oxygen in arterial blood, which may or may not result in visible cyanosis depending on hemoglobin levels and oxygen saturation. The major difference lies in that cyanosis is a physical manifestation detectable during examination, while hypoxemia is a measurable laboratory value obtained from arterial blood gas analysis.
Clinical Manifestations: Recognizing Signs and Symptoms
Cyanosis presents as a bluish discoloration of the skin and mucous membranes, primarily visible in the lips, tongue, and nail beds, indicating deoxygenated hemoglobin above 5 g/dL. Hypoxemia refers to low arterial oxygen partial pressure (PaO2 below 80 mm Hg) and may not always result in cyanosis, especially in cases of anemia or peripheral vasodilation. Clinical manifestations of hypoxemia include tachypnea, dyspnea, confusion, and tachycardia, highlighting oxygen deficiency before visible cyanotic changes occur.
Pathophysiology: Underlying Mechanisms
Cyanosis results from increased levels of deoxygenated hemoglobin (>5 g/dL) in the capillary blood, leading to a bluish discoloration of the skin and mucous membranes. Hypoxemia denotes reduced partial pressure of oxygen (PaO2) in arterial blood, causing systemic oxygen deficiency at the tissue level. While hypoxemia can induce cyanosis, factors like anemia or abnormal hemoglobin variants can cause cyanosis without hypoxemia, highlighting distinct yet overlapping pathophysiological mechanisms.
Diagnostic Approaches for Cyanosis and Hypoxemia
Diagnostic approaches for cyanosis involve clinical assessment of the blue discoloration of the skin and mucous membranes, often confirmed by pulse oximetry to detect low oxygen saturation levels. Hypoxemia diagnosis primarily relies on arterial blood gas (ABG) analysis to measure partial pressure of oxygen (PaO2) and oxygen saturation directly, providing precise quantification of oxygen deficiency in blood. Both conditions require evaluation of underlying causes through chest X-rays, echocardiography, and pulmonary function tests to differentiate respiratory or cardiac origins.
Common Causes: Diseases and Conditions
Cyanosis commonly arises from conditions such as chronic obstructive pulmonary disease (COPD), congenital heart defects, and severe pneumonia, which impair oxygen delivery to tissues. Hypoxemia is frequently caused by diseases like pulmonary embolism, acute respiratory distress syndrome (ARDS), and high-altitude exposure that reduce arterial oxygen saturation. Both conditions reflect underlying respiratory or cardiovascular dysfunction but differ in their clinical presentation and specific pathophysiology.
Treatment Strategies: Addressing the Underlying Issues
Treatment strategies for cyanosis center on correcting the underlying causes such as congenital heart defects or respiratory disorders to restore adequate oxygenation. Hypoxemia management involves oxygen therapy, mechanical ventilation, and addressing conditions like pneumonia or chronic obstructive pulmonary disease to improve blood oxygen levels. Both conditions require targeted interventions including medication, surgery, or lifestyle modifications based on precise diagnosis to effectively alleviate symptoms and prevent complications.
Prognosis and Complications
Prognosis of cyanosis depends on the underlying cause, with central cyanosis often indicating serious cardiopulmonary conditions requiring prompt intervention to prevent organ damage. Hypoxemia, characterized by low arterial oxygen levels, can lead to complications such as pulmonary hypertension, right heart failure, and cognitive impairment if untreated. Both conditions necessitate early diagnosis and management to improve clinical outcomes and reduce long-term morbidity.
Prevention and Patient Education
Effective prevention of cyanosis and hypoxemia involves regular monitoring of oxygen saturation levels using pulse oximetry and managing underlying respiratory or cardiovascular conditions promptly. Patient education should emphasize recognizing early symptoms such as bluish skin discoloration, shortness of breath, and fatigue, as well as the importance of avoiding smoking, exposure to high altitudes, and pollutants that can exacerbate hypoxemia. Proper use of prescribed oxygen therapy and adherence to medication regimens significantly reduce the risk of severe complications related to inadequate oxygen delivery.
Cyanosis Infographic
 libterm.com
libterm.com