Hemorrhage occurs when blood vessels rupture, leading to excessive blood loss either internally or externally, which can be life-threatening if not treated promptly. Understanding the causes, symptoms, and emergency responses to hemorrhage is crucial for effective management and prevention of complications. Explore this article to learn how you can recognize and respond to hemorrhage situations swiftly.
Table of Comparison
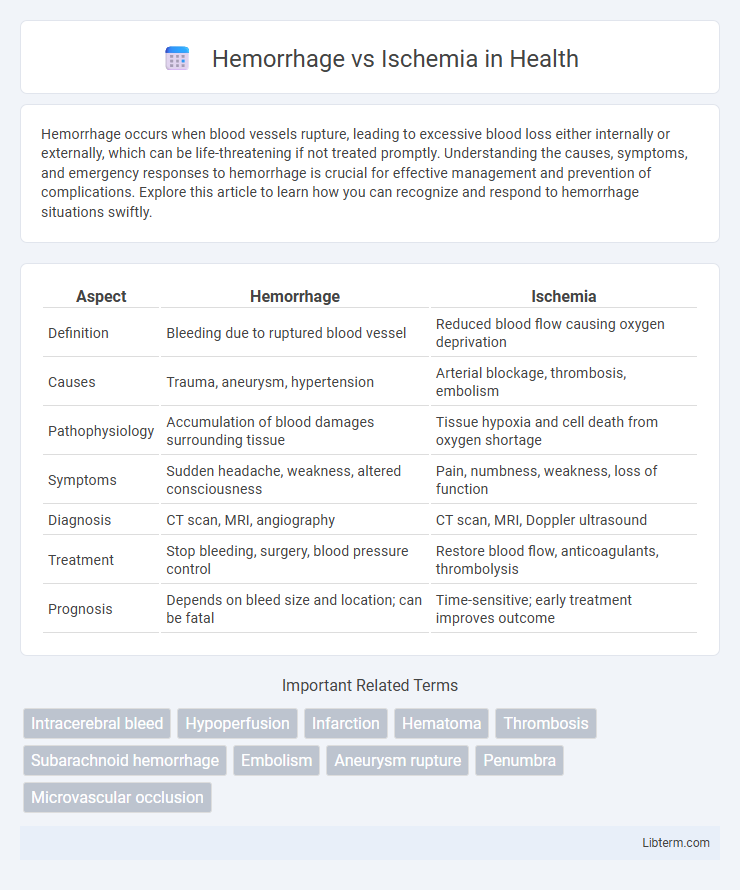
| Aspect | Hemorrhage | Ischemia |
|---|---|---|
| Definition | Bleeding due to ruptured blood vessel | Reduced blood flow causing oxygen deprivation |
| Causes | Trauma, aneurysm, hypertension | Arterial blockage, thrombosis, embolism |
| Pathophysiology | Accumulation of blood damages surrounding tissue | Tissue hypoxia and cell death from oxygen shortage |
| Symptoms | Sudden headache, weakness, altered consciousness | Pain, numbness, weakness, loss of function |
| Diagnosis | CT scan, MRI, angiography | CT scan, MRI, Doppler ultrasound |
| Treatment | Stop bleeding, surgery, blood pressure control | Restore blood flow, anticoagulants, thrombolysis |
| Prognosis | Depends on bleed size and location; can be fatal | Time-sensitive; early treatment improves outcome |
Introduction to Hemorrhage and Ischemia
Hemorrhage refers to the escape of blood from a ruptured blood vessel, leading to internal or external bleeding that can cause tissue damage and dysfunction. Ischemia is characterized by insufficient blood flow to tissues, resulting in oxygen deprivation and cellular injury. Both conditions disrupt normal tissue perfusion but differ fundamentally in their underlying mechanisms and clinical implications.
Defining Hemorrhage: Causes and Types
Hemorrhage is the escape of blood from ruptured blood vessels, leading to external or internal bleeding that disrupts tissue oxygenation and function. Common causes include trauma, hypertension, aneurysm rupture, and coagulation disorders, with types classified as intracranial, gastrointestinal, and subcutaneous hemorrhages. Understanding the specific hemorrhage type aids in targeted diagnosis and treatment to prevent severe complications such as stroke or organ failure.
Understanding Ischemia: Mechanisms and Triggers
Ischemia occurs when blood flow to tissues is restricted, leading to oxygen deprivation and cell damage. Key mechanisms include arterial occlusion from atherosclerosis, embolism, or thrombosis, resulting in insufficient oxygen and nutrient delivery. Common triggers involve sudden arterial blockages, low blood pressure, or vessel spasms that compromise tissue perfusion and cause metabolic stress.
Key Differences Between Hemorrhage and Ischemia
Hemorrhage involves bleeding caused by blood vessel rupture, leading to blood accumulation and increased intracranial pressure, whereas ischemia results from blood flow obstruction, depriving tissues of oxygen and nutrients. Hemorrhage often presents with sudden headache, neurological deficits, and hematoma formation, while ischemia typically manifests as gradual neurological impairment or stroke due to tissue hypoxia. Diagnosis relies on imaging techniques like CT for hemorrhage detection and MRI or cerebral angiography for ischemia assessment.
Risk Factors for Hemorrhage and Ischemia
Hemorrhage risk factors include hypertension, anticoagulant use, vascular malformations, and trauma, increasing the likelihood of blood vessel rupture. Ischemia risk factors primarily involve atherosclerosis, diabetes, smoking, and atrial fibrillation, which contribute to blood flow obstruction and tissue oxygen deprivation. Both conditions share age and high cholesterol as common risk factors, impacting overall cerebrovascular health.
Clinical Manifestations and Symptoms
Hemorrhage often presents with sudden severe headache, nausea, vomiting, altered consciousness, and focal neurological deficits due to intracranial bleeding and increased intracranial pressure. Ischemia typically manifests as sudden weakness or numbness on one side of the body, difficulty speaking, vision disturbances, and confusion resulting from reduced blood flow and oxygen delivery to brain tissue. Both conditions require rapid diagnosis, but hemorrhage symptoms generally develop more abruptly and with greater severity compared to the more variable presentation of ischemia.
Diagnostic Approaches: Hemorrhage vs Ischemia
Diagnostic approaches for hemorrhage commonly involve non-contrast CT scans to quickly identify bleeding and hematoma location, while ischemia diagnosis typically relies on diffusion-weighted MRI to detect early infarcted brain tissue. Blood tests, including coagulation profiles, aid in hemorrhage evaluation, whereas ischemia assessment may incorporate vascular imaging like CT angiography or MR angiography to visualize occluded vessels. Prompt differentiation between hemorrhagic and ischemic stroke through imaging is critical for guiding appropriate treatment strategies and improving patient outcomes.
Treatment Strategies and Emergency Management
Hemorrhage treatment prioritizes controlling bleeding through surgical intervention or embolization, while ischemia demands rapid restoration of blood flow via thrombolytics, angioplasty, or thrombectomy. Emergency management for hemorrhage often includes fluid resuscitation and blood transfusion to maintain hemodynamic stability, whereas ischemic events necessitate oxygen therapy and anticoagulants to prevent clot extension. Both conditions require continuous monitoring of neurological status and vital signs to guide timely therapeutic adjustments.
Prognosis and Long-Term Outcomes
Hemorrhage typically results in worse immediate prognosis due to increased intracranial pressure and risk of rebleeding, often leading to more severe neurological deficits compared to ischemia. Ischemic stroke outcomes vary widely depending on the extent of brain tissue affected, with some patients experiencing significant recovery due to neuroplasticity and effective reperfusion therapies. Long-term outcomes for hemorrhagic strokes generally involve higher mortality and disability rates, while ischemic strokes have better potential for rehabilitation and functional improvement.
Prevention and Patient Education
Preventing hemorrhage involves controlling hypertension, avoiding anticoagulant misuse, and managing trauma risks, while ischemia prevention focuses on maintaining cardiovascular health through diet, exercise, and controlling diabetes or hyperlipidemia. Patient education should emphasize recognizing early warning signs such as sudden weakness, speech difficulties, or severe headaches, and the importance of timely medical intervention. Empowering patients with lifestyle modification knowledge and adherence to prescribed medications significantly reduces the incidence and severity of both hemorrhagic and ischemic events.
Hemorrhage Infographic
 libterm.com
libterm.com