Narcolepsy and hypersomnia are neurological disorders characterized by excessive daytime sleepiness and disrupted nighttime sleep patterns. These conditions impact your daily functioning, causing sudden sleep attacks or prolonged sleep episodes that interfere with work, relationships, and safety. Explore the rest of the article to understand the symptoms, causes, and effective treatments for managing these sleep disorders.
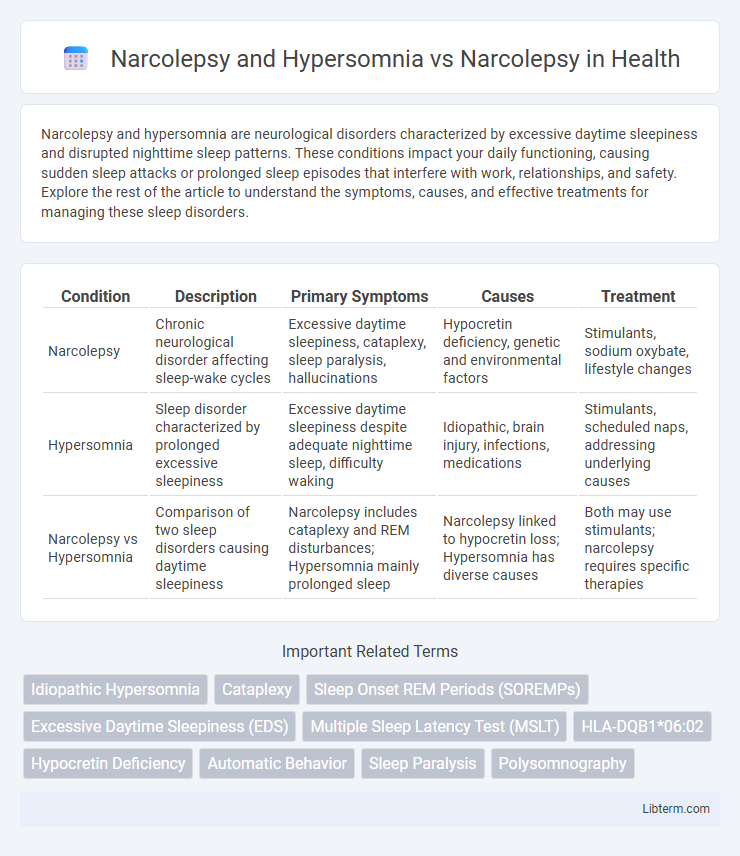
Table of Comparison
| Condition | Description | Primary Symptoms | Causes | Treatment |
|---|---|---|---|---|
| Narcolepsy | Chronic neurological disorder affecting sleep-wake cycles | Excessive daytime sleepiness, cataplexy, sleep paralysis, hallucinations | Hypocretin deficiency, genetic and environmental factors | Stimulants, sodium oxybate, lifestyle changes |
| Hypersomnia | Sleep disorder characterized by prolonged excessive sleepiness | Excessive daytime sleepiness despite adequate nighttime sleep, difficulty waking | Idiopathic, brain injury, infections, medications | Stimulants, scheduled naps, addressing underlying causes |
| Narcolepsy vs Hypersomnia | Comparison of two sleep disorders causing daytime sleepiness | Narcolepsy includes cataplexy and REM disturbances; Hypersomnia mainly prolonged sleep | Narcolepsy linked to hypocretin loss; Hypersomnia has diverse causes | Both may use stimulants; narcolepsy requires specific therapies |
Understanding Narcolepsy: Definition and Symptoms
Narcolepsy is a chronic neurological disorder characterized by excessive daytime sleepiness and sudden muscle weakness called cataplexy, distinguishing it from hypersomnia, which primarily involves prolonged sleep duration without the sudden episodes. Key symptoms of narcolepsy include sleep paralysis, hypnagogic hallucinations, and disrupted nighttime sleep, whereas hypersomnia focuses on difficulty staying awake despite adequate or extended night rest. Understanding the distinct features of narcolepsy aids in accurate diagnosis and targeted treatment, optimizing patient care and quality of life.
What is Hypersomnia? Key Features and Diagnosis
Hypersomnia is a neurological disorder characterized by excessive daytime sleepiness despite sufficient or prolonged nighttime sleep, often causing impaired daily functioning. Key features include prolonged nighttime sleep, difficulty waking, excessive daytime sleep episodes, and non-restorative naps, distinguishing it from narcolepsy, which involves cataplexy and sleep paralysis. Diagnosis involves polysomnography and Multiple Sleep Latency Test (MSLT) to measure sleep onset latency and REM sleep episodes, helping differentiate hypersomnia from narcolepsy and other sleep disorders.
Narcolepsy vs Hypersomnia: Core Differences
Narcolepsy is a chronic neurological disorder characterized by excessive daytime sleepiness, cataplexy, sleep paralysis, and hallucinations, whereas hypersomnia primarily involves prolonged sleep duration and difficulty staying awake without the distinct symptoms of narcolepsy. Narcolepsy results from hypocretin (orexin) deficiency in the brain, disrupting the sleep-wake cycle, while hypersomnia often stems from underlying conditions like sleep apnea, depression, or medication effects. Diagnostic criteria differentiate narcolepsy by the presence of REM sleep abnormalities on polysomnography and multiple sleep latency tests, unlike hypersomnia, which lacks these hallmark features.
Shared Symptoms: Narcolepsy and Hypersomnia Overlap
Narcolepsy and hypersomnia share several overlapping symptoms, including excessive daytime sleepiness (EDS), sudden sleep attacks, and disruptions in nighttime sleep patterns. Both conditions can lead to cognitive impairment, memory difficulties, and reduced quality of life due to persistent fatigue and sleep fragmentation. Accurate diagnosis requires distinguishing narcolepsy's hallmark cataplexy and sleep paralysis from hypersomnia's prolonged sleep duration and difficulty waking.
Underlying Causes: Exploring Neurological Mechanisms
Narcolepsy results from the loss of hypocretin-producing neurons in the hypothalamus, causing impaired regulation of the sleep-wake cycle and excessive daytime sleepiness. Hypersomnia primarily involves abnormalities in brain regions linked to arousal and sleep homeostasis, with potential genetic and metabolic influences affecting neurotransmitter systems like GABA and dopamine. Understanding these distinct neurological mechanisms aids in differentiating narcolepsy from other hypersomnia disorders and guides targeted treatment approaches.
Impact on Daily Life and Functioning
Narcolepsy and Hypersomnia both significantly disrupt daily life by causing excessive daytime sleepiness, but Narcolepsy includes sudden muscle weakness or cataplexy, leading to more unpredictable social and occupational challenges. Hypersomnia primarily involves prolonged nighttime sleep and persistent fatigue, affecting concentration and productivity but without the abrupt loss of muscle control seen in Narcolepsy. Managing Narcolepsy often requires careful planning to mitigate the impact of sudden sleep attacks, while Hypersomnia management focuses on improving overall sleep quality and maintaining alertness throughout the day.
Diagnostic Criteria: Narcolepsy vs Hypersomnia
Narcolepsy diagnostic criteria emphasize excessive daytime sleepiness with cataplexy or hypocretin deficiency, confirmed by multiple sleep latency test showing sleep onset REM periods. Hypersomnia diagnosis requires persistent excessive daytime sleepiness not explained by narcolepsy, including criteria like prolonged nocturnal sleep or recurrent sleep episodes without REM abnormalities. Differentiating narcolepsy from hypersomnia relies on polysomnographic evidence and clinical features such as cataplexy and sleep-onset REM latency.
Treatment Options and Management Strategies
Treatment options for narcolepsy and hypersomnia vary based on symptom severity and underlying causes, with narcolepsy often managed through stimulants like modafinil, sodium oxybate, and pitolisant to reduce excessive daytime sleepiness and cataplexy. Hypersomnia treatment may include wake-promoting agents such as modafinil or methylphenidate, alongside lifestyle modifications like structured sleep schedules and cognitive-behavioral therapy to improve sleep quality. Management strategies emphasize individualized care plans involving sleep hygiene education, scheduled naps, and regular follow-up with sleep specialists to optimize daytime functioning and quality of life.
Long-Term Outlook and Prognosis Comparison
Narcolepsy and hypersomnia both involve excessive daytime sleepiness but differ significantly in long-term outlook and prognosis. Narcolepsy, characterized by sudden sleep attacks and cataplexy, often requires lifelong symptom management with medications like modafinil and sodium oxybate to improve quality of life. Idiopathic hypersomnia generally shows a more stable course with less severe symptoms but may also necessitate ongoing treatment to manage persistent drowsiness and impaired alertness.
Living with Narcolepsy or Hypersomnia: Patient Perspectives
Living with narcolepsy or hypersomnia involves managing excessive daytime sleepiness that disrupts daily activities and social interactions. Patients often describe challenges such as sudden sleep attacks and difficulty maintaining regular schedules, which impact quality of life and emotional well-being. Effective treatment plans combining medication and behavioral strategies are crucial for improving symptoms and supporting patient coping mechanisms.
Narcolepsy and Hypersomnia Infographic
 libterm.com
libterm.com