Angiogenesis is the physiological process through which new blood vessels form from pre-existing vessels, playing a critical role in growth, wound healing, and tissue regeneration. This process is tightly regulated by various chemical signals, such as vascular endothelial growth factor (VEGF), and is essential for maintaining healthy tissues as well as contributing to disease progression like cancer. Explore the rest of the article to understand how angiogenesis impacts your health and modern medical treatments.
Table of Comparison
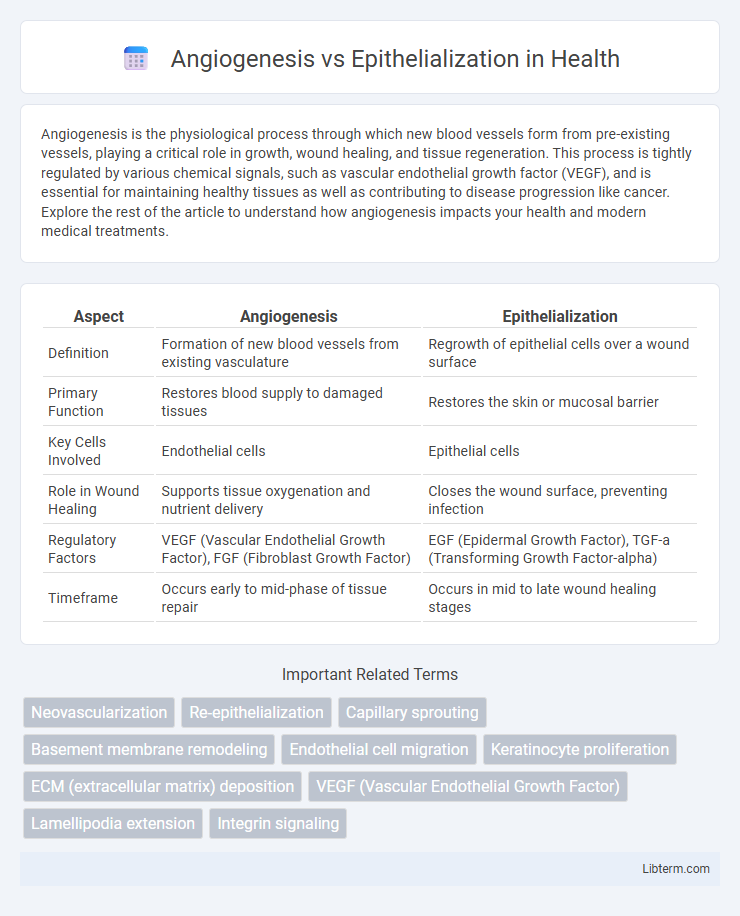
| Aspect | Angiogenesis | Epithelialization |
|---|---|---|
| Definition | Formation of new blood vessels from existing vasculature | Regrowth of epithelial cells over a wound surface |
| Primary Function | Restores blood supply to damaged tissues | Restores the skin or mucosal barrier |
| Key Cells Involved | Endothelial cells | Epithelial cells |
| Role in Wound Healing | Supports tissue oxygenation and nutrient delivery | Closes the wound surface, preventing infection |
| Regulatory Factors | VEGF (Vascular Endothelial Growth Factor), FGF (Fibroblast Growth Factor) | EGF (Epidermal Growth Factor), TGF-a (Transforming Growth Factor-alpha) |
| Timeframe | Occurs early to mid-phase of tissue repair | Occurs in mid to late wound healing stages |
Understanding Angiogenesis: Key Mechanisms
Angiogenesis involves the formation of new blood vessels from pre-existing vasculature, driven by key mechanisms such as endothelial cell proliferation, migration, and differentiation, regulated by growth factors like VEGF (vascular endothelial growth factor) and FGF (fibroblast growth factor). This process is critical for wound healing and tissue regeneration, supplying oxygen and nutrients essential for cellular survival and function. In contrast, epithelialization is the migration and proliferation of epithelial cells to cover wound surfaces, a process that depends on effective angiogenesis to support the metabolic demands of new tissue formation.
The Process of Epithelialization Explained
Epithelialization is a critical phase in wound healing characterized by the migration and proliferation of epithelial cells across the wound bed to restore the skin barrier. This process involves keratinocytes moving from the wound edges and hair follicles, guided by growth factors such as epidermal growth factor (EGF) and transforming growth factor-alpha (TGF-a). Unlike angiogenesis, which forms new blood vessels to supply nutrients, epithelialization primarily focuses on reestablishing the protective epithelial layer, ensuring wound closure and barrier function.
Cellular Players in Angiogenesis
Angiogenesis involves endothelial cells, pericytes, and fibroblasts coordinating to form new blood vessels from existing vasculature, driven by growth factors such as VEGF and FGF. Endothelial cells proliferate, migrate, and organize into tubular structures while pericytes stabilize and mature the nascent vessels. In contrast, epithelialization primarily involves keratinocytes migrating and proliferating to restore the epithelial barrier during wound healing.
Epithelialization: Involved Cells and Functions
Epithelialization primarily involves keratinocytes, which migrate, proliferate, and differentiate to restore the epithelial barrier after injury, ensuring wound closure. Epidermal stem cells play a critical role by replenishing keratinocytes, while Langerhans cells contribute to immunological defense during this process. The coordinated action of growth factors like EGF and TGF-b regulates cellular proliferation and migration, facilitating tissue regeneration and barrier restoration.
Molecular Pathways: Angiogenesis vs Epithelialization
Angiogenesis involves the VEGF (vascular endothelial growth factor) signaling pathway, which activates endothelial cells to promote new blood vessel formation through PI3K/Akt and MAPK cascades. Epithelialization is primarily regulated by the EGF (epidermal growth factor) pathway, triggering keratinocyte proliferation and migration via the Ras/Raf/MEK/ERK signaling axis. Both processes integrate cytokines and growth factors but engage distinct molecular mechanisms vital for wound healing.
Sequential Phases in Wound Healing
Angiogenesis and epithelialization are critical sequential phases in wound healing, where angiogenesis involves the formation of new blood vessels to supply nutrients and oxygen, promoting tissue regeneration. This phase typically occurs during the proliferative stage, facilitating the migration and proliferation of epithelial cells in the subsequent epithelialization phase that restores the skin barrier. Efficient coordination between these processes accelerates tissue repair and reduces the risk of chronic wounds.
Clinical Significance of Angiogenesis
Angiogenesis plays a critical role in wound healing by forming new blood vessels, which supply essential oxygen and nutrients to regenerating tissues, thus accelerating recovery. Clinically, impaired or excessive angiogenesis can lead to chronic wounds or pathological conditions like cancer and diabetic ulcers, making it a key target for therapeutic intervention. Enhancing angiogenesis through growth factors such as VEGF (vascular endothelial growth factor) improves epithelialization indirectly by supporting the underlying vascular network necessary for tissue regeneration.
Role of Epithelialization in Tissue Repair
Epithelialization plays a critical role in tissue repair by restoring the integrity of the skin or mucosal surfaces through the proliferation and migration of epithelial cells over the wound bed. This process re-establishes the protective barrier, preventing infection and fluid loss while facilitating underlying tissue regeneration. Epithelialization often follows angiogenesis, which supplies oxygen and nutrients essential for effective wound healing and tissue remodeling.
Therapeutic Strategies Targeting Angiogenesis and Epithelialization
Therapeutic strategies targeting angiogenesis focus on promoting or inhibiting new blood vessel formation to enhance wound healing or treat diseases like cancer and diabetic ulcers. Approaches include growth factor delivery such as VEGF, gene therapy, and biomaterials designed to stimulate vascular regeneration. In contrast, therapies targeting epithelialization aim to accelerate epithelial cell migration and proliferation using agents like EGF and keratinocyte growth factors, often combined with scaffolds to restore skin barrier integrity effectively.
Comparing Angiogenesis and Epithelialization: Key Differences and Interactions
Angiogenesis involves the formation of new blood vessels from pre-existing vasculature, critical for supplying oxygen and nutrients during tissue repair, whereas epithelialization refers to the migration and proliferation of epithelial cells to cover a wound surface, restoring the skin barrier. These processes differ in cellular mechanisms and functions: angiogenesis depends on endothelial cell proliferation and vascular endothelial growth factor (VEGF) signaling, while epithelialization relies on keratinocyte movement and epidermal growth factor (EGF) pathways. Despite distinct roles, angiogenesis supports epithelialization by enhancing nutrient delivery, and the interplay between these processes is essential for efficient wound healing and tissue regeneration.
Angiogenesis Infographic
 libterm.com
libterm.com