Empyema is a collection of pus in the pleural cavity, often resulting from bacterial infections, while tuberculosis is a chronic infectious disease caused by Mycobacterium tuberculosis primarily affecting the lungs. Both conditions can cause severe respiratory symptoms and require timely diagnosis and treatment to prevent complications. Explore the rest of the article to understand the differences, symptoms, diagnosis, and treatment options for empyema and tuberculosis.
Table of Comparison
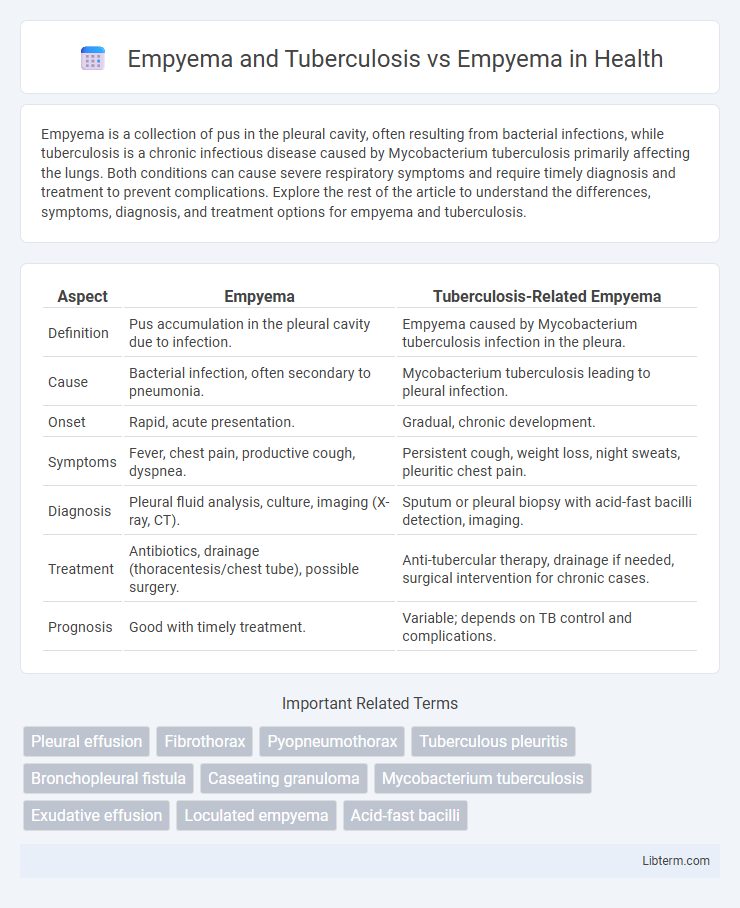
| Aspect | Empyema | Tuberculosis-Related Empyema |
|---|---|---|
| Definition | Pus accumulation in the pleural cavity due to infection. | Empyema caused by Mycobacterium tuberculosis infection in the pleura. |
| Cause | Bacterial infection, often secondary to pneumonia. | Mycobacterium tuberculosis leading to pleural infection. |
| Onset | Rapid, acute presentation. | Gradual, chronic development. |
| Symptoms | Fever, chest pain, productive cough, dyspnea. | Persistent cough, weight loss, night sweats, pleuritic chest pain. |
| Diagnosis | Pleural fluid analysis, culture, imaging (X-ray, CT). | Sputum or pleural biopsy with acid-fast bacilli detection, imaging. |
| Treatment | Antibiotics, drainage (thoracentesis/chest tube), possible surgery. | Anti-tubercular therapy, drainage if needed, surgical intervention for chronic cases. |
| Prognosis | Good with timely treatment. | Variable; depends on TB control and complications. |
Introduction to Empyema
Empyema is the accumulation of pus within the pleural cavity, often arising from bacterial infections or complications of pneumonia. In contrast, empyema associated with tuberculosis typically results from Mycobacterium tuberculosis infection causing chronic pleural inflammation and loculated pus. Understanding the distinct pathophysiology of tuberculous versus non-tuberculous empyema is crucial for accurate diagnosis and targeted treatment strategies.
Understanding Tuberculosis
Empyema caused by tuberculosis results from the infection of the pleural space by Mycobacterium tuberculosis, leading to chronic pus accumulation and pleural thickening. Tuberculous empyema differs from non-tuberculous empyema by its slower progression, resistance to routine antibiotics, and frequent association with active pulmonary tuberculosis. Understanding tuberculosis is critical for diagnosing and managing empyema, as treatment requires prolonged anti-tubercular therapy combined with drainage to prevent complications and improve patient outcomes.
Pathophysiology of Empyema
Empyema, characterized by the accumulation of pus in the pleural space, results from bacterial infection leading to inflammation, fibrin deposition, and loculation. In tuberculosis-associated empyema, Mycobacterium tuberculosis induces a chronic granulomatous response with caseous necrosis and pleural thickening, differentiating it from the acute bacterial etiology seen in non-tuberculous empyema. Pathophysiological changes in both forms disrupt pleural fluid resorption and promote fibrotic remodeling, complicating lung re-expansion and requiring targeted antimicrobial and sometimes surgical intervention.
Etiology: Tuberculosis-Related vs Non-Tuberculous Empyema
Empyema linked to tuberculosis is characterized by Mycobacterium tuberculosis infection causing pleural space pus accumulation, often following primary pulmonary tuberculosis or reactivation. Non-tuberculous empyema primarily results from bacterial pathogens such as Streptococcus pneumoniae, Staphylococcus aureus, or anaerobes, frequently due to pneumonia, thoracic surgery, or trauma. Differentiating etiology through pleural fluid analysis and microbiological cultures is crucial for targeted antimicrobial and antitubercular therapy.
Clinical Presentation: Empyema vs Tuberculous Empyema
Empyema typically presents with acute symptoms such as high fever, pleuritic chest pain, productive cough, and dyspnea, reflecting bacterial infection and pus accumulation in the pleural space. Tuberculous empyema often manifests more insidiously with chronic symptoms including low-grade fever, night sweats, weight loss, and a longer duration of pleural inflammation related to Mycobacterium tuberculosis infection. The clinical differentiation relies on the acuity and systemic features, where tuberculous empyema shows protracted illness and constitutional symptoms compared to the rapid progression seen in pyogenic empyema.
Diagnostic Approaches
Empyema diagnosis involves imaging techniques such as chest X-ray, ultrasound, and CT scan to identify pleural effusions and assess fluid characteristics, supplemented by thoracentesis for fluid analysis and microbiological culture. Tuberculous empyema requires additional diagnostic approaches including sputum smear microscopy, Mycobacterium tuberculosis culture, and nucleic acid amplification tests (NAATs) to detect tuberculosis infection specifically. Pleural biopsy and interferon-gamma release assays (IGRAs) enhance diagnostic accuracy in differentiating tuberculous empyema from non-tuberculous empyema cases.
Radiological Differences
Radiologically, empyema presents as a pleural effusion with loculated fluid collections, thickened enhancing pleura, and split pleura sign on contrast-enhanced CT, indicating infected pleural space. Tuberculous empyema often exhibits calcified pleural plaques, multiloculated effusions, and associated parenchymal abnormalities such as upper lobe cavitary lesions or fibrotic changes typical of tuberculosis. In contrast, non-tuberculous empyema usually lacks pleural calcification and demonstrates more uniform pleural thickening without the distinct pulmonary fibrosis or cavitations seen in tuberculosis.
Treatment Strategies: Standard Empyema vs TB Empyema
Standard empyema treatment typically involves thoracentesis or chest tube drainage combined with broad-spectrum antibiotics targeting common bacterial pathogens. In TB empyema, management requires prolonged anti-tubercular therapy alongside surgical drainage due to the granulomatous nature of Mycobacterium tuberculosis infection. Early surgical intervention, such as decortication, is more frequently necessary in TB empyema to resolve thick pleural peels and ensure lung re-expansion, contrasting with the often less invasive approach in non-tuberculous empyema.
Prognosis and Complications
Empyema associated with Tuberculosis often leads to a more complex prognosis due to the chronic nature of Mycobacterium tuberculosis infection, resulting in prolonged inflammation and fibrosis, which may cause restrictive lung disease. In comparison, non-tuberculous empyema typically has a better prognosis with appropriate antibiotic therapy and drainage, although complications such as bronchopleural fistula and sepsis remain concerns. Tuberculous empyema poses a higher risk of pleural thickening, trapped lung, and relapse, significantly impacting patient morbidity and requiring extended treatment duration.
Prevention and Public Health Considerations
Empyema associated with tuberculosis requires targeted prevention strategies including timely diagnosis and adherence to anti-tubercular treatment to reduce disease progression and transmission. Vaccination with Bacillus Calmette-Guerin (BCG) and public health measures such as improved sanitation, early screening, and contact tracing are critical in controlling tuberculosis-related empyema. In contrast, prevention of non-tuberculous empyema centers on prompt management of bacterial pneumonia, vaccination against Streptococcus pneumoniae and Haemophilus influenzae, and minimizing risk factors like smoking and immunosuppression.
Empyema and Tuberculosis Infographic
 libterm.com
libterm.com