Excess oxygen exposure, known as hyperoxia, can cause oxidative stress leading to cellular damage and inflammation in the lungs and other organs. Prolonged hyperoxia may result in complications such as acute lung injury, impaired tissue repair, and neurological effects. Explore the article to understand the risks, symptoms, and management strategies of hyperoxia for your health and safety.
Table of Comparison
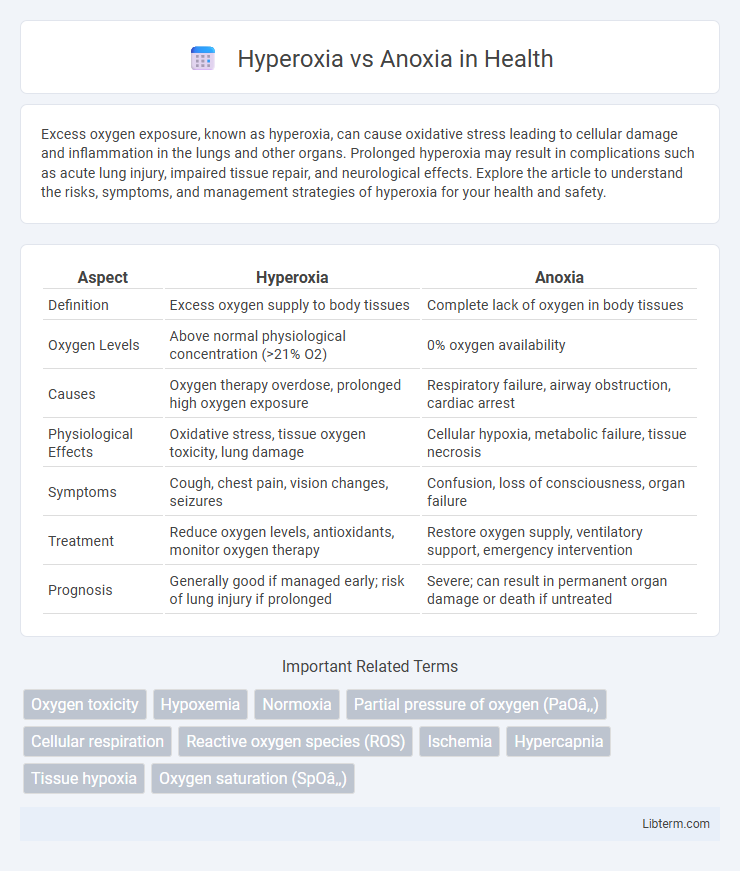
| Aspect | Hyperoxia | Anoxia |
|---|---|---|
| Definition | Excess oxygen supply to body tissues | Complete lack of oxygen in body tissues |
| Oxygen Levels | Above normal physiological concentration (>21% O2) | 0% oxygen availability |
| Causes | Oxygen therapy overdose, prolonged high oxygen exposure | Respiratory failure, airway obstruction, cardiac arrest |
| Physiological Effects | Oxidative stress, tissue oxygen toxicity, lung damage | Cellular hypoxia, metabolic failure, tissue necrosis |
| Symptoms | Cough, chest pain, vision changes, seizures | Confusion, loss of consciousness, organ failure |
| Treatment | Reduce oxygen levels, antioxidants, monitor oxygen therapy | Restore oxygen supply, ventilatory support, emergency intervention |
| Prognosis | Generally good if managed early; risk of lung injury if prolonged | Severe; can result in permanent organ damage or death if untreated |
Introduction to Hyperoxia and Anoxia
Hyperoxia refers to a condition where tissues and organs are exposed to an excessive supply of oxygen, often above the normal atmospheric level, leading to oxidative stress and potential cellular damage. Anoxia denotes the complete absence of oxygen in tissues, causing severe metabolic disruption and cell death due to halted aerobic respiration. Both conditions critically influence cellular homeostasis and require precise medical management to prevent tissue injury and ensure survival.
Defining Hyperoxia: Causes and Mechanisms
Hyperoxia occurs when tissues are exposed to oxygen levels exceeding normal atmospheric concentration, typically above 21% O2. Common causes include supplemental oxygen therapy, hyperbaric oxygen treatment, and prolonged exposure to high-oxygen environments. The mechanisms involve increased partial pressure of oxygen, leading to elevated reactive oxygen species (ROS) generation, oxidative stress, and potential cellular damage.
Understanding Anoxia: Etiology and Pathophysiology
Anoxia results from the complete absence of oxygen supply to tissues, leading to cellular injury and eventual death due to energy failure caused by impaired oxidative phosphorylation. Etiological factors include airway obstruction, severe anemia, carbon monoxide poisoning, and ischemia, each disrupting oxygen delivery or utilization at the cellular level. Pathophysiologically, anoxia triggers a cascade of metabolic disturbances such as ATP depletion, accumulation of reactive oxygen species, and initiation of apoptosis or necrosis depending on the duration and severity of oxygen deprivation.
Key Differences Between Hyperoxia and Anoxia
Hyperoxia occurs when tissues are exposed to excess oxygen levels, often leading to oxygen toxicity, while anoxia is the complete absence of oxygen supply to tissues, causing severe cellular damage and potential cell death. Hyperoxia typically results in oxidative stress and damage to lung and eye tissues, whereas anoxia triggers metabolic failure and necrosis due to insufficient oxygen for aerobic respiration. The critical difference lies in oxygen availability: hyperoxia involves oxygen overload, often from medical oxygen therapy, whereas anoxia results from interrupted blood flow or airway obstruction leading to total oxygen deprivation.
Physiological Effects of Excess Oxygen (Hyperoxia)
Hyperoxia, characterized by elevated oxygen levels beyond normal physiological concentrations, induces oxidative stress through excessive reactive oxygen species (ROS) production, leading to cellular and tissue damage. This condition can impair pulmonary function by causing alveolar inflammation, vasoconstriction, and potential acute lung injury, while also disrupting central nervous system activity resulting in symptoms such as seizures and altered neural signaling. Prolonged hyperoxia exposure adversely affects mitochondrial function, exacerbates apoptosis, and compromises organ systems, contrasting sharply with anoxia, which is defined by a complete lack of oxygen leading to ischemic injury.
Consequences of Oxygen Deprivation (Anoxia)
Oxygen deprivation, or anoxia, leads to severe cellular damage, particularly in brain tissue where neurons rely heavily on oxidative metabolism for energy production. Prolonged anoxia causes irreversible neuronal death, resulting in cognitive impairments, loss of motor function, and potentially fatal outcomes such as brain infarction or stroke. Unlike hyperoxia, which may generate oxidative stress, anoxia critically disrupts ATP synthesis, causing cell membrane failure and triggering apoptosis or necrosis.
Clinical Manifestations: Hyperoxia vs Anoxia
Hyperoxia commonly presents with symptoms such as oxygen toxicity leading to lung damage, central nervous system disturbances including seizures, and visual impairment due to retinopathy, particularly in neonates. Anoxia results in rapid tissue hypoxia manifesting clinically as confusion, loss of consciousness, cyanosis, and if prolonged, irreversible brain damage or cardiac arrest. Distinguishing clinical manifestations between hyperoxia and anoxia is critical for appropriate oxygen therapy management in critical care settings.
Diagnostic Approaches for Oxygen Imbalance
Diagnostic approaches for oxygen imbalance differentiate hyperoxia and anoxia by measuring oxygen partial pressure using pulse oximetry and arterial blood gas analysis. Hyperoxia is identified by elevated arterial oxygen tension (PaO2) above normal physiological levels, while anoxia is characterized by severely reduced or absent oxygen levels in tissues. Imaging techniques such as MRI and near-infrared spectroscopy (NIRS) can assess tissue oxygenation, assisting in precise diagnosis and management of oxygen-related disorders.
Therapeutic Interventions and Management Strategies
Therapeutic interventions for hyperoxia prioritize reducing oxygen exposure to prevent oxidative stress and cellular damage, often utilizing controlled oxygen therapy and antioxidant administration. Management strategies for anoxia focus on restoring oxygen delivery rapidly through supplemental oxygen, mechanical ventilation, and addressing underlying causes such as airway obstruction or cardiac arrest. Both conditions require careful monitoring of oxygen levels with pulse oximetry and arterial blood gases to tailor treatment and minimize tissue injury.
Prevention and Risk Reduction: Best Practices
Effective prevention of hyperoxia involves closely monitoring oxygen therapy to maintain optimal saturation levels, avoiding excessive oxygen delivery that can lead to oxidative stress and tissue damage. Reducing the risk of anoxia requires ensuring uninterrupted oxygen supply, prompt recognition of hypoxic symptoms, and timely intervention to restore adequate oxygenation to tissues. Implementing standardized protocols for oxygen administration and continuous patient assessment are critical best practices to minimize complications from both hyperoxia and anoxia.
Hyperoxia Infographic
 libterm.com
libterm.com