Peribronchial refers to the area surrounding the bronchi, the large airways in the lungs that conduct air in and out. Inflammation or thickening of the peribronchial tissues can indicate conditions such as bronchitis, asthma, or infections. Discover how peribronchial changes impact lung health and what symptoms to watch for in the following article.
Table of Comparison
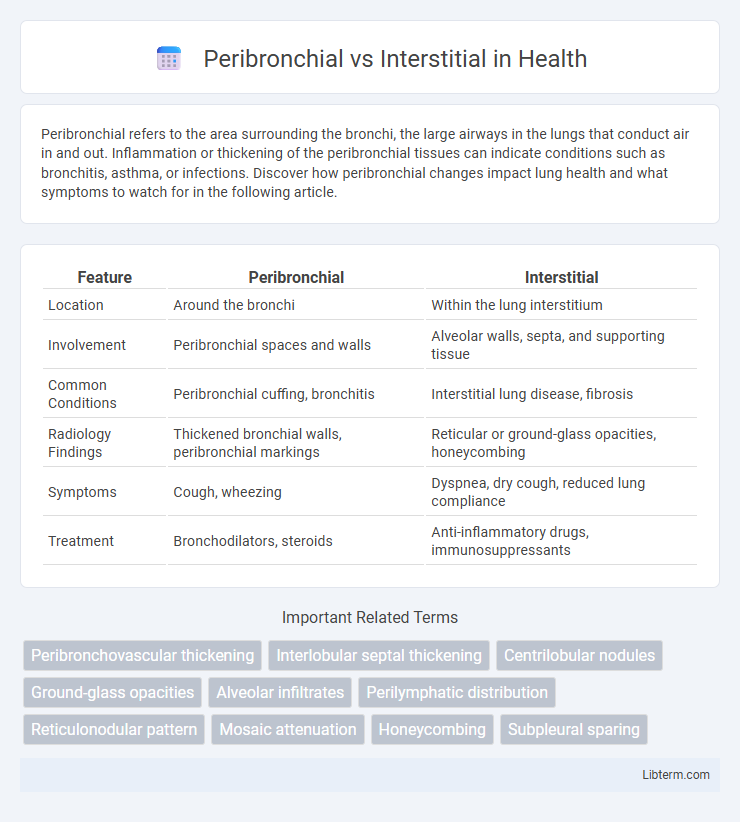
| Feature | Peribronchial | Interstitial |
|---|---|---|
| Location | Around the bronchi | Within the lung interstitium |
| Involvement | Peribronchial spaces and walls | Alveolar walls, septa, and supporting tissue |
| Common Conditions | Peribronchial cuffing, bronchitis | Interstitial lung disease, fibrosis |
| Radiology Findings | Thickened bronchial walls, peribronchial markings | Reticular or ground-glass opacities, honeycombing |
| Symptoms | Cough, wheezing | Dyspnea, dry cough, reduced lung compliance |
| Treatment | Bronchodilators, steroids | Anti-inflammatory drugs, immunosuppressants |
Understanding Peribronchial and Interstitial Patterns
Peribronchial patterns involve abnormalities centered around the bronchial walls, often indicating inflammation or fibrosis surrounding the airways, visible as thickened bronchial walls on imaging. Interstitial patterns refer to changes within the lung interstitium, including the alveolar walls and supporting structures, commonly presenting as reticular or nodular opacities, which reflect conditions such as pulmonary fibrosis or interstitial pneumonias. Differentiating peribronchial from interstitial patterns is crucial for accurate diagnosis and management of lung diseases, as each pattern correlates with distinct pathological processes and clinical outcomes.
Anatomy of the Bronchi and Interstitium
Peribronchial tissue surrounds the bronchi, consisting primarily of connective tissue, smooth muscle fibers, and lymphatic channels that support airflow regulation and immune defense within the bronchial walls. The bronchi themselves are tubular structures lined with pseudostratified ciliated columnar epithelium, cartilage plates for structural integrity, and submucosal glands producing mucus. In contrast, the interstitial space refers to the connective tissue framework between alveoli, composed of collagen and elastin fibers, capillaries, fibroblasts, and immune cells, which provides structural support and facilitates gas exchange by maintaining the lung parenchyma's architecture.
Radiologic Features: Peribronchial vs Interstitial Involvement
Peribronchial involvement on radiologic imaging typically presents as thickening or cuffing around the bronchi, often seen on chest X-rays and CT scans as linear or nodular opacities following bronchial walls. Interstitial involvement is characterized by diffuse reticular, reticulonodular, or ground-glass patterns affecting the lung interstitium, visible primarily on high-resolution CT as a network of fine lines or nodules between alveoli. Distinguishing peribronchial from interstitial changes aids in diagnosing underlying conditions such as bronchitis, bronchiectasis for peribronchial, and interstitial lung diseases like idiopathic pulmonary fibrosis or sarcoidosis for interstitial involvement.
Common Causes of Peribronchial Changes
Peribronchial changes commonly result from chronic bronchitis, asthma, and infectious bronchopneumonia, leading to thickening around the bronchi due to inflammation or fibrosis. Interstitial changes, in contrast, typically involve the lung parenchyma itself and are seen in conditions like pulmonary fibrosis, sarcoidosis, and interstitial lung diseases. Identifying peribronchial thickening on imaging helps differentiate airway-centered diseases from diffuse interstitial processes.
Common Causes of Interstitial Changes
Interstitial changes in the lungs commonly arise from infections such as viral pneumonia and atypical bacterial infections like Mycoplasma pneumoniae, which affect the lung interstitium rather than the airways. Other frequent causes include interstitial lung diseases (ILD) such as idiopathic pulmonary fibrosis, sarcoidosis, and hypersensitivity pneumonitis, characterized by inflammation and fibrosis affecting the lung interstitium. Occupational exposures to asbestos, silica, and other inhaled irritants also contribute significantly to interstitial changes by inducing chronic inflammation and scarring in the lung interstitial tissue.
Symptoms Associated with Each Pattern
Peribronchial patterns often present with symptoms such as chronic cough, wheezing, and shortness of breath due to airway inflammation and obstruction. Interstitial patterns typically cause progressive dyspnea, dry cough, and restrictive lung function linked to fibrosis and alveolar damage. Differentiating these patterns is crucial for targeted diagnosis and treatment of underlying pulmonary conditions.
Diagnostic Approaches and Imaging Techniques
Peribronchial and interstitial lung diseases require distinct diagnostic approaches, with high-resolution computed tomography (HRCT) being the cornerstone imaging technique for differentiation. Peribronchial abnormalities typically present as thickening or cuffing around the bronchi, visible on HRCT as concentric opacities, while interstitial diseases often manifest as diffuse reticular patterns or ground-glass opacities reflecting fibrosis or inflammation within the lung interstitium. Additional diagnostic tools include pulmonary function tests and bronchoalveolar lavage, which help correlate imaging findings with functional impairment and inflammatory cell profiles.
Treatment Strategies: Peribronchial vs Interstitial Disease
Peribronchial disease often requires targeted anti-inflammatory or bronchodilator therapies to reduce airway inflammation and improve airflow, while interstitial disease treatment primarily focuses on antifibrotic agents and immunosuppressants to slow fibrosis progression and preserve lung function. In peribronchial conditions, corticosteroids and bronchodilators like beta-agonists are commonly used to manage symptoms and prevent exacerbations. Interstitial lung disease management may include drugs such as pirfenidone or nintedanib, along with oxygen therapy and pulmonary rehabilitation to enhance quality of life.
Prognostic Differences and Clinical Outcomes
Peribronchial involvement typically indicates inflammation or fibrosis concentrated around the bronchi, often associated with better prognostic outcomes compared to interstitial patterns, which involve diffuse lung parenchyma and correlate with more severe functional impairment. Interstitial lung disease shows a higher risk for progressive lung function decline, increased morbidity, and poorer survival rates due to extensive alveolar damage and fibrosis. Accurate differentiation through imaging and histopathology is crucial for tailoring treatment and predicting patient prognosis in pulmonary disorders.
Summary: Key Differences and Clinical Relevance
Peribronchial involvement primarily affects the walls surrounding the bronchi, often seen in conditions like bronchitis and asthma, characterized by airway inflammation and thickening. Interstitial changes occur within the lung parenchyma's supporting tissue, typical of interstitial lung diseases such as idiopathic pulmonary fibrosis, marked by fibrosis and impaired gas exchange. Clinically, distinguishing between peribronchial and interstitial patterns aids in accurate diagnosis, guiding appropriate treatment strategies and prognosis assessment.
Peribronchial Infographic
 libterm.com
libterm.com