Achalasia is a rare esophageal disorder characterized by the inability of the lower esophageal sphincter to relax, leading to difficulty swallowing and food accumulation in the esophagus. This condition often causes symptoms such as chest pain, regurgitation, and weight loss, requiring accurate diagnosis and effective management. Discover how you can recognize the signs, understand available treatments, and improve your quality of life by reading the full article.
Table of Comparison
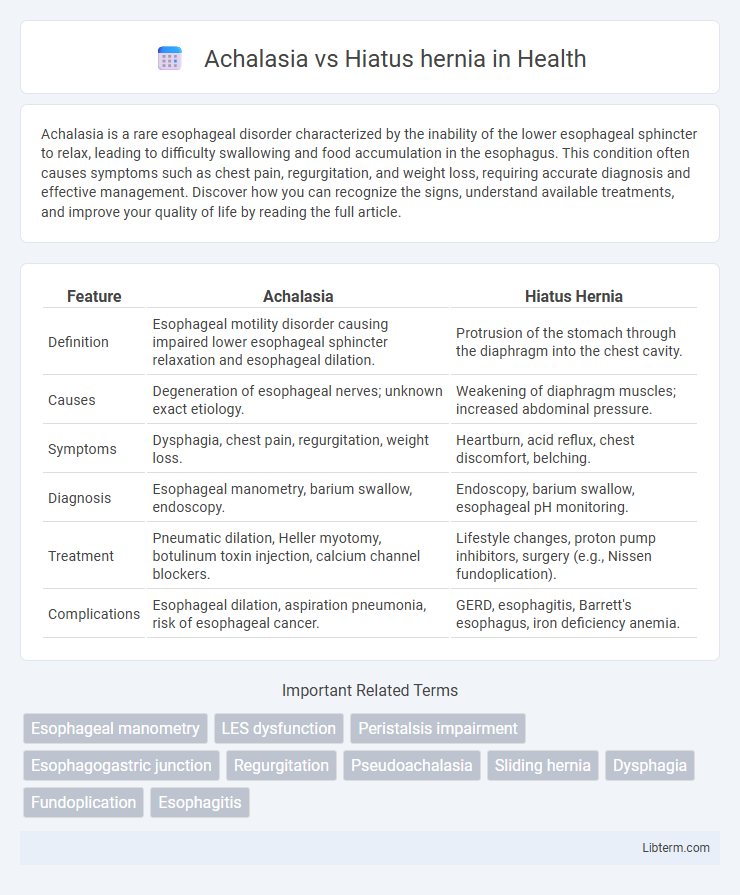
| Feature | Achalasia | Hiatus Hernia |
|---|---|---|
| Definition | Esophageal motility disorder causing impaired lower esophageal sphincter relaxation and esophageal dilation. | Protrusion of the stomach through the diaphragm into the chest cavity. |
| Causes | Degeneration of esophageal nerves; unknown exact etiology. | Weakening of diaphragm muscles; increased abdominal pressure. |
| Symptoms | Dysphagia, chest pain, regurgitation, weight loss. | Heartburn, acid reflux, chest discomfort, belching. |
| Diagnosis | Esophageal manometry, barium swallow, endoscopy. | Endoscopy, barium swallow, esophageal pH monitoring. |
| Treatment | Pneumatic dilation, Heller myotomy, botulinum toxin injection, calcium channel blockers. | Lifestyle changes, proton pump inhibitors, surgery (e.g., Nissen fundoplication). |
| Complications | Esophageal dilation, aspiration pneumonia, risk of esophageal cancer. | GERD, esophagitis, Barrett's esophagus, iron deficiency anemia. |
Introduction to Achalasia and Hiatus Hernia
Achalasia is a rare esophageal motility disorder characterized by the inability of the lower esophageal sphincter to relax, leading to difficulty in swallowing (dysphagia) and food stasis. Hiatus hernia occurs when part of the stomach protrudes through the esophageal hiatus of the diaphragm into the chest cavity, often causing gastroesophageal reflux symptoms. Both conditions affect the esophagus but differ in pathophysiology, with achalasia primarily involving nerve dysfunction and hiatus hernia involving anatomical displacement.
Understanding Achalasia: Causes and Risk Factors
Achalasia is a rare esophageal motility disorder caused by the degeneration of neurons in the esophageal myenteric plexus, leading to impaired relaxation of the lower esophageal sphincter (LES) and disrupted peristalsis. Primary achalasia lacks a defined cause but may involve autoimmune mechanisms, while secondary achalasia results from infections, malignancies, or Chagas disease. Risk factors include age between 25 and 60 years, family history, and exposure to certain viral agents, distinguishing it from hiatus hernia, which primarily involves the anatomical displacement of the stomach through the diaphragm.
Overview of Hiatus Hernia: Types and Triggers
Hiatus hernia occurs when part of the stomach pushes through the diaphragm into the chest cavity, primarily classified into sliding and paraesophageal types. Sliding hiatus hernia is the most common, characterized by the stomach and lower esophageal sphincter moving above the diaphragm, often triggered by factors such as obesity, age-related muscle weakening, and excessive intra-abdominal pressure. Paraesophageal hernia, less common but more serious, involves part of the stomach herniating alongside the esophagus, with potential triggers including trauma and chronic coughing.
Key Differences Between Achalasia and Hiatus Hernia
Achalasia is a primary esophageal motility disorder characterized by the failure of the lower esophageal sphincter (LES) to relax and the absence of esophageal peristalsis, leading to difficulty swallowing and food retention. Hiatus hernia involves the protrusion of the stomach through the diaphragmatic esophageal hiatus into the chest, often causing gastroesophageal reflux symptoms like heartburn and regurgitation. Unlike achalasia's functional obstruction, hiatus hernia is an anatomical anomaly, diagnosed primarily through endoscopy and imaging studies such as barium swallow or CT scan.
Common Symptoms: Achalasia vs Hiatus Hernia
Achalasia typically presents with dysphagia, regurgitation of undigested food, and chest pain due to impaired esophageal motility and LES relaxation. Hiatus hernia commonly causes heartburn, acid reflux, and chest discomfort resulting from stomach acid refluxing into the esophagus through the displaced gastroesophageal junction. Both conditions may cause chest pain and swallowing difficulties, but achalasia symptoms are more related to esophageal motility dysfunction, while hiatus hernia symptoms primarily arise from gastroesophageal reflux.
Diagnostic Approaches for Achalasia and Hiatus Hernia
Diagnostic approaches for achalasia primarily include esophageal manometry, which measures the pressure and coordination of esophageal muscles, and barium swallow radiography that reveals a characteristic "bird beak" narrowing at the lower esophageal sphincter. In contrast, hiatus hernia diagnosis relies heavily on upper endoscopy (esophagogastroduodenoscopy) to visualize the herniation of the stomach through the diaphragm and on imaging techniques such as chest X-ray or barium swallow to confirm anatomical displacement. High-resolution manometry remains the gold standard for achalasia differentiation, while radiographic evidence and endoscopic findings are essential for identifying hiatus hernia and its complications.
Treatment Options for Achalasia
Treatment options for achalasia primarily include pneumatic dilation, laparoscopic Heller myotomy, and peroral endoscopic myotomy (POEM), aiming to relieve esophageal sphincter pressure and improve swallowing. Botox injections offer temporary relief by relaxing the lower esophageal sphincter but are less effective long-term. Surgical interventions like Heller myotomy combined with partial fundoplication reduce reflux risk, while medical management with calcium channel blockers or nitrates is reserved for patients unable to undergo procedural treatments.
Hiatus Hernia Management and Therapies
Hiatus hernia management primarily involves lifestyle modifications such as weight loss, elevating the head during sleep, and dietary changes to reduce reflux symptoms. Pharmacological therapies include proton pump inhibitors (PPIs) and H2 receptor antagonists to decrease gastric acid production and alleviate esophageal irritation. In severe cases, surgical options like laparoscopic Nissen fundoplication can restore the function of the lower esophageal sphincter and prevent hernia recurrence.
Complications and Long-Term Outlook
Achalasia can lead to complications such as esophageal dilation, aspiration pneumonia, and increased risk of esophageal cancer due to chronic stasis and inflammation. Hiatus hernia complications often include gastroesophageal reflux disease (GERD), esophagitis, and in severe cases, strangulation or obstruction of the stomach. The long-term outlook for achalasia involves managing symptoms with interventions like pneumatic dilation or myotomy, while hiatus hernia prognosis improves significantly with lifestyle changes, medications, and surgical repair when necessary.
Preventive Strategies and Lifestyle Recommendations
Preventive strategies for achalasia primarily focus on early diagnosis and managing risk factors such as autoimmune conditions, whereas hiatus hernia prevention emphasizes maintaining a healthy body weight and avoiding activities that increase abdominal pressure, like heavy lifting or straining during bowel movements. Lifestyle recommendations for achalasia include eating smaller, more frequent meals and avoiding foods that trigger symptoms, while hiatus hernia management advises elevating the head during sleep, avoiding large meals before bedtime, and reducing intake of caffeine, alcohol, and acidic foods. Both conditions benefit from smoking cessation and stress management to reduce symptom severity and improve overall esophageal health.
Achalasia Infographic
 libterm.com
libterm.com