Inflammation is the body's natural response to injury or infection, aiming to protect and heal affected tissues. Chronic inflammation, however, can contribute to various diseases, including arthritis, heart disease, and diabetes. Discover how managing inflammation can improve your overall health by exploring the rest of this article.
Table of Comparison
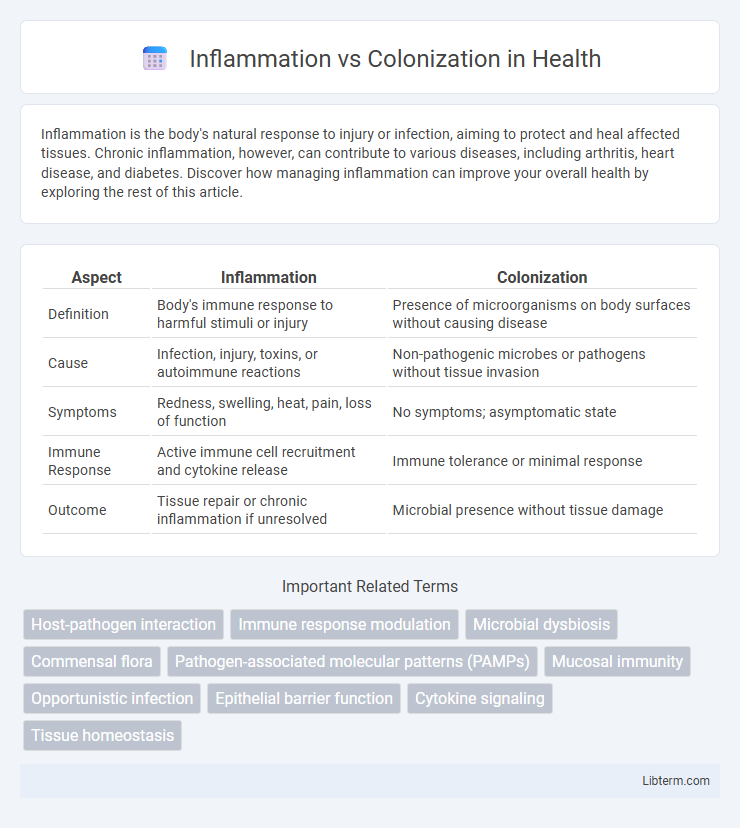
| Aspect | Inflammation | Colonization |
|---|---|---|
| Definition | Body's immune response to harmful stimuli or injury | Presence of microorganisms on body surfaces without causing disease |
| Cause | Infection, injury, toxins, or autoimmune reactions | Non-pathogenic microbes or pathogens without tissue invasion |
| Symptoms | Redness, swelling, heat, pain, loss of function | No symptoms; asymptomatic state |
| Immune Response | Active immune cell recruitment and cytokine release | Immune tolerance or minimal response |
| Outcome | Tissue repair or chronic inflammation if unresolved | Microbial presence without tissue damage |
Understanding Inflammation and Colonization
Inflammation is the body's immune response to harmful stimuli, characterized by redness, swelling, heat, and pain as it aims to eliminate pathogens and initiate tissue repair. Colonization refers to the presence and growth of microorganisms on body surfaces without causing tissue damage or an immune response. Differentiating between inflammation and colonization is crucial in clinical diagnosis to avoid unnecessary treatments and accurately target infections.
Key Definitions: Inflammation vs Colonization
Inflammation is the body's immune response to harmful stimuli such as pathogens, injury, or toxins, characterized by redness, swelling, heat, pain, and loss of function. Colonization refers to the presence and growth of microorganisms on a surface or tissue without causing an immune response or tissue damage. Understanding the distinction between inflammation and colonization is crucial for diagnosing infections and determining appropriate medical treatments.
Causes and Triggers of Inflammation
Inflammation is primarily triggered by the immune system's response to harmful stimuli such as pathogens, tissue injury, or chemical irritants, aiming to eliminate the cause and initiate healing. Colonization, on the other hand, refers to the presence of microorganisms on a body surface without provoking inflammation or immune activation. Key causes of inflammation include bacterial infections, physical damage, autoimmune reactions, and exposure to toxins, which activate immune cells and release pro-inflammatory cytokines like interleukins and tumor necrosis factor-alpha.
Microbial Colonization Explained
Microbial colonization refers to the natural process where microorganisms establish themselves on body surfaces without causing harm or triggering an immune response, differing significantly from inflammation, which is the body's protective reaction to infection or injury. Colonization involves a balanced interaction between host and microbes, often contributing to health by supporting digestion and preventing pathogen overgrowth. Understanding microbial colonization helps distinguish harmless microbial presence from harmful infections that prompt inflammatory responses.
Immune Response: How the Body Reacts
Inflammation triggers a complex immune response involving the activation of white blood cells, release of cytokines, and increased blood flow to the affected tissue, aiming to eliminate pathogens and initiate healing. Colonization occurs when microorganisms reside on or within the body without eliciting such an immune activation, maintaining a balanced interaction with host defenses. The distinction lies in inflammation signaling an active defense mechanism, whereas colonization represents a steady-state coexistence with minimal immune disruption.
Clinical Signs: Differentiating Inflammation from Colonization
Clinical signs of inflammation include redness, swelling, heat, pain, and loss of function at the affected site, indicating an active immune response to infection or injury. Colonization, in contrast, often shows no clinical symptoms as microorganisms are present without tissue invasion or immune activation. Differentiating between inflammation and colonization is crucial for accurate diagnosis and appropriate treatment, as colonization does not always require antimicrobial therapy.
Diagnostic Approaches and Tools
Diagnostic approaches for inflammation typically involve biomarkers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) alongside imaging techniques like MRI and ultrasound to assess tissue swelling and immune response. Colonization detection relies on microbial culture methods, polymerase chain reaction (PCR), and next-generation sequencing (NGS) to identify and quantify colonizing bacteria without signs of host inflammation. Differentiating between inflammation and colonization requires integrating clinical presentation with laboratory results to guide accurate diagnosis and appropriate treatment strategies.
Impact on Disease Progression and Health
Inflammation triggers immune responses that can exacerbate tissue damage and accelerate disease progression, whereas colonization by non-pathogenic microbes may promote immune system balance and protect against infections. Persistent inflammation in diseases like inflammatory bowel disease (IBD) leads to chronic tissue injury, whereas controlled colonization supports mucosal barrier integrity and overall gut health. Understanding the distinct roles of inflammation and colonization is crucial for developing targeted therapies that mitigate disease while preserving beneficial microbial populations.
Treatment Strategies: Managing Both Conditions
Treatment strategies for inflammation prioritize anti-inflammatory medications such as corticosteroids and NSAIDs to reduce tissue damage and immune response, while colonization management focuses on targeted antimicrobial therapy to inhibit bacterial growth without triggering resistance. Combining probiotics and prebiotics can support gut microbiota balance, enhancing colonization control and reducing inflammation. Early diagnostic differentiation between inflammation and colonization improves personalized therapy, minimizing overtreatment and promoting effective symptom resolution.
Prevention and Future Research Directions
Preventing inflammation and colonization requires targeted strategies such as maintaining gut microbiota balance, using probiotics, and implementing early diagnostic biomarkers to detect asymptomatic colonization. Future research should explore the molecular mechanisms underlying host-pathogen interactions and develop novel anti-inflammatory agents alongside advanced microbiome modulation techniques. Emphasis on personalized medicine approaches and high-throughput sequencing technologies will drive breakthroughs in managing colonization without triggering harmful inflammatory responses.
Inflammation Infographic
 libterm.com
libterm.com