Infection occurs when harmful microorganisms like bacteria, viruses, or fungi invade the body, triggering immune responses and symptoms ranging from mild discomfort to severe illness. Understanding the types, causes, and prevention methods is crucial for effective treatment and maintaining your health. Explore the rest of the article to learn how to identify, manage, and prevent infections effectively.
Table of Comparison
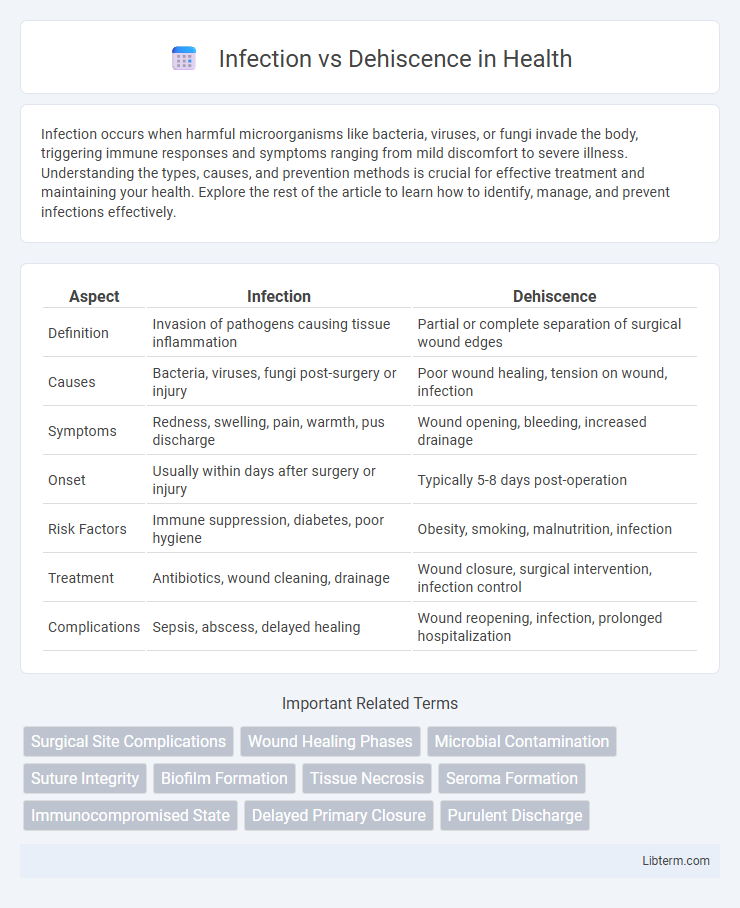
| Aspect | Infection | Dehiscence |
|---|---|---|
| Definition | Invasion of pathogens causing tissue inflammation | Partial or complete separation of surgical wound edges |
| Causes | Bacteria, viruses, fungi post-surgery or injury | Poor wound healing, tension on wound, infection |
| Symptoms | Redness, swelling, pain, warmth, pus discharge | Wound opening, bleeding, increased drainage |
| Onset | Usually within days after surgery or injury | Typically 5-8 days post-operation |
| Risk Factors | Immune suppression, diabetes, poor hygiene | Obesity, smoking, malnutrition, infection |
| Treatment | Antibiotics, wound cleaning, drainage | Wound closure, surgical intervention, infection control |
| Complications | Sepsis, abscess, delayed healing | Wound reopening, infection, prolonged hospitalization |
Introduction: Understanding Infection and Dehiscence
Infection and dehiscence are critical complications affecting wound healing and surgical recovery. Infection involves the invasion of pathogens causing tissue inflammation and systemic symptoms, while dehiscence refers to the partial or complete reopening of a surgical incision. Differentiating between these conditions ensures timely intervention, reducing morbidity and improving patient outcomes.
Defining Infection in Surgical and Wound Care
Infection in surgical and wound care refers to the invasion and multiplication of pathogenic microorganisms within the wound site, causing inflammation and delayed healing. It is characterized by signs such as redness, swelling, warmth, pain, and purulent discharge, which distinguish it from dehiscence, a mechanical separation of wound edges. Understanding and identifying infection is critical for timely intervention to prevent complications like systemic sepsis and impaired tissue repair.
What is Dehiscence? Meaning and Clinical Context
Dehiscence refers to the partial or complete separation of a surgical wound along its sutured edges, commonly occurring in post-operative patients. This complication compromises wound integrity, increasing susceptibility to infection and prolonged healing times. Clinical context often involves risk factors such as poor surgical technique, infection, malnutrition, or excessive tension on the wound edges.
Causes and Risk Factors: Infection vs Dehiscence
Infection is primarily caused by bacterial contamination during or after surgery, with risk factors including poor hygiene, immunosuppression, and prolonged operative time. Dehiscence results from mechanical failure of wound closure, often linked to factors such as obesity, excessive tension on wound edges, diabetes, and inadequate surgical technique. Both conditions are more likely in patients with malnutrition, chronic illness, or compromised immune response, increasing the complexity of postoperative recovery.
Clinical Signs and Symptoms to Differentiate
Infection typically presents with localized redness, swelling, warmth, pain, and purulent discharge at the wound site, often accompanied by systemic signs such as fever and malaise. Dehiscence is characterized by the partial or complete separation of wound edges, resulting in visible wound opening without necessarily having purulent discharge or systemic infection signs. Differentiating factors include the presence of purulent fluid and systemic symptoms in infection, while dehiscence primarily involves mechanical wound disruption with possible serosanguinous exudate but minimal inflammatory signs.
Diagnostic Approaches: Identifying Infection and Dehiscence
Diagnostic approaches for infection involve microbiological cultures, blood tests for elevated inflammatory markers such as C-reactive protein and white blood cell count, and imaging techniques including ultrasound or MRI to detect abscess formation. Dehiscence diagnosis primarily relies on physical examination, noting wound separation and exposure of underlying tissues, supported by wound measurement and serial photographic documentation to monitor progression. Combining clinical assessment with targeted imaging and laboratory tests enhances accuracy in distinguishing infection from wound dehiscence for timely intervention.
Treatment Strategies: Infection vs Dehiscence Management
Infection management involves prompt antibiotic therapy guided by culture sensitivity, wound debridement, and maintaining sterile dressing changes to prevent systemic spread. Dehiscence treatment focuses on wound stabilization through suturing or supportive dressings, ensuring adequate nutrition, and monitoring for underlying causes such as infection or increased tension on the wound site. Both conditions require close clinical evaluation, but infection necessitates antimicrobial intervention, while dehiscence prioritizes mechanical wound support and prevention of further tissue separation.
Prevention Tips: Reducing Risk of Both Conditions
Maintaining strict wound hygiene by regularly cleaning and dressing the site can significantly reduce the risk of infection and dehiscence. Using sterile techniques during surgical procedures and promoting proper nutrition rich in protein and vitamins supports tissue healing and immune function. Monitoring for early signs of wound complications enables prompt intervention, preventing progression to severe infection or wound separation.
Complications and Prognosis: Impact on Healing
Infection in surgical wounds often leads to delayed healing due to bacterial colonization that triggers inflammation and tissue damage, increasing the risk of systemic complications like sepsis. Dehiscence, characterized by the partial or complete separation of wound edges, frequently results from excessive tension, poor surgical technique, or infection and delays tissue regeneration by exposing the wound to contamination. Both complications significantly impair prognosis by prolonging recovery time, elevating morbidity rates, and potentially necessitating secondary interventions such as reoperation or extended antibiotic therapy.
Conclusion: Key Takeaways on Infection vs Dehiscence
Infection involves the invasion of pathogens leading to inflammation and delayed wound healing, while dehiscence refers to the partial or complete reopening of a surgical incision. Effective wound management requires early identification of signs such as purulent discharge for infection and wound gap or separation for dehiscence. Prompt intervention with antibiotics for infection and surgical repair for dehiscence is critical to prevent severe complications and ensure optimal recovery.
Infection Infographic
 libterm.com
libterm.com