Intracranial tumors are abnormal growths located within the brain or surrounding tissues that can disrupt normal neurological function and cause symptoms like headaches, seizures, or cognitive changes. Early detection and accurate diagnosis are crucial for effective treatment, which may include surgery, radiation therapy, or chemotherapy depending on the tumor type and location. Explore the rest of this article to understand the complexities of intracranial tumors and how they might impact your health.
Table of Comparison
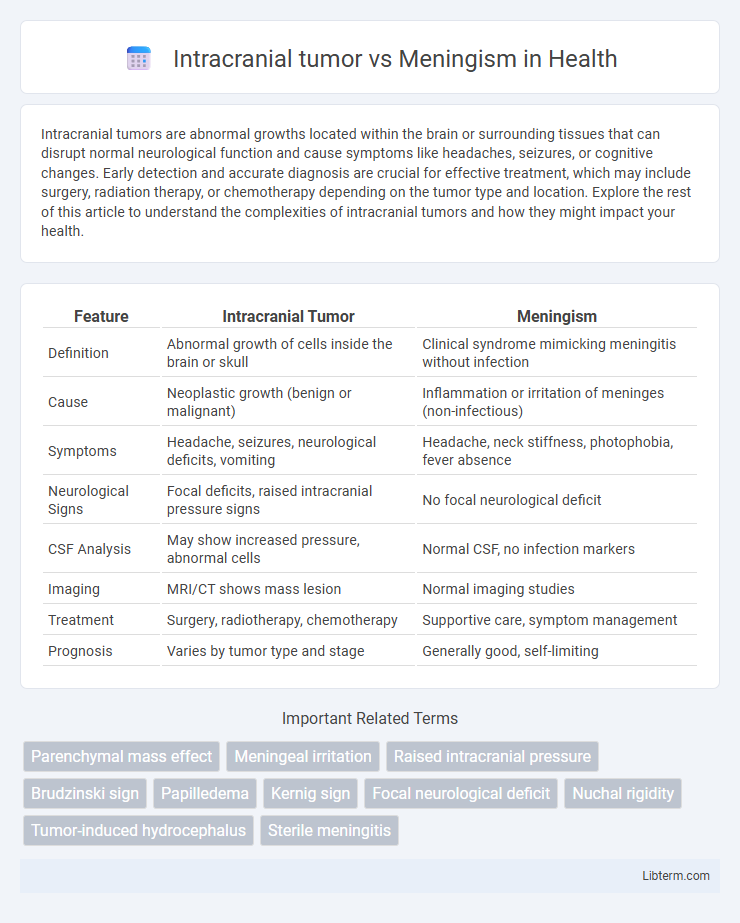
| Feature | Intracranial Tumor | Meningism |
|---|---|---|
| Definition | Abnormal growth of cells inside the brain or skull | Clinical syndrome mimicking meningitis without infection |
| Cause | Neoplastic growth (benign or malignant) | Inflammation or irritation of meninges (non-infectious) |
| Symptoms | Headache, seizures, neurological deficits, vomiting | Headache, neck stiffness, photophobia, fever absence |
| Neurological Signs | Focal deficits, raised intracranial pressure signs | No focal neurological deficit |
| CSF Analysis | May show increased pressure, abnormal cells | Normal CSF, no infection markers |
| Imaging | MRI/CT shows mass lesion | Normal imaging studies |
| Treatment | Surgery, radiotherapy, chemotherapy | Supportive care, symptom management |
| Prognosis | Varies by tumor type and stage | Generally good, self-limiting |
Introduction: Understanding Intracranial Tumor and Meningism
Intracranial tumors are abnormal growths within the skull that can disrupt brain function and cause symptoms such as headaches, seizures, and neurological deficits. Meningism refers to clinical signs resembling meningitis, including neck stiffness, photophobia, and headache, without evidence of meningeal infection. Differentiating between intracranial tumors and meningism is critical for accurate diagnosis and targeted treatment strategies.
Definition and Overview
Intracranial tumors are abnormal growths of cells within the brain or surrounding structures, often causing neurological deficits due to pressure on adjacent tissues. Meningism refers to a set of symptoms including neck stiffness, photophobia, and headache that mimic meningitis but occur without actual inflammation of the meninges. Differentiating between intracranial tumors and meningism is crucial for accurate diagnosis and treatment, as tumors require imaging and possible surgical intervention, while meningism often indicates benign or infectious processes.
Etiology: Causes of Intracranial Tumor and Meningism
Intracranial tumors primarily arise from genetic mutations leading to uncontrolled cell proliferation in brain tissues, with gliomas, meningiomas, and metastatic lesions being common types. Meningism results from inflammation or irritation of the meninges, often caused by infections such as viral or bacterial meningitis, subarachnoid hemorrhage, or autoimmune conditions. Distinguishing these etiologies is crucial for diagnosis, as intracranial tumors involve tumor growth while meningism stems from meningeal irritation without tumor presence.
Epidemiology and Risk Factors
Intracranial tumors present with diverse epidemiological patterns, predominantly affecting adults aged 45-70, with gliomas representing the most common subtype, while meningiomas are more frequent in females, especially those exposed to ionizing radiation. Meningism, often resulting from infectious or inflammatory causes, is most prevalent among children and young adults, with risk factors including recent upper respiratory infections and immunosuppression. Both conditions are influenced by genetic predispositions, but intracranial tumors show stronger associations with environmental carcinogens, whereas meningism correlates more with contagious pathogens and systemic inflammatory states.
Pathophysiology: Mechanisms Behind Each Condition
Intracranial tumors cause pathophysiological changes primarily through mass effect, increased intracranial pressure, and disruption of normal brain tissue architecture, leading to neurological deficits. Meningism results from meningeal irritation without actual inflammation, characterized by heightened sensitivity of the meninges and activation of pain receptors, typically due to infections or systemic illness. The distinction lies in the tumor's direct structural impact versus meningism's functional irritation-driven mechanisms.
Clinical Presentation: Signs and Symptoms Comparison
Intracranial tumors commonly present with progressive headaches, focal neurological deficits, seizures, and signs of increased intracranial pressure such as nausea, vomiting, and papilledema. Meningism typically manifests with neck stiffness, photophobia, headache, and symptoms resembling meningeal irritation without actual infection or intracranial mass lesions. Unlike intracranial tumors, meningism's neurological examination is usually normal except for meningeal signs like positive Kernig and Brudzinski signs.
Diagnostic Approach and Key Differences
Intracranial tumors typically present with focal neurological deficits, altered mental status, and signs of increased intracranial pressure, while meningism manifests with neck stiffness, photophobia, and headache without focal neurological signs. Diagnostic imaging such as MRI or CT scans are essential for identifying intracranial tumors, whereas meningism diagnosis relies on clinical examination and cerebrospinal fluid analysis via lumbar puncture to exclude infections or inflammation. Key differences include the presence of tumor mass effect and radiologic abnormalities in intracranial tumors, contrasted with meningeal irritation signs and normal brain imaging in meningism cases.
Imaging and Laboratory Investigations
Intracranial tumors typically exhibit abnormal mass lesions with contrast enhancement and perilesional edema on MRI or CT scans, whereas meningism shows no such focal lesions but may present with meningeal enhancement if associated with inflammation. Cerebrospinal fluid (CSF) analysis in intracranial tumors often reveals elevated protein levels and sometimes malignant cells, while meningism is characterized by pleocytosis, elevated white blood cell count, and normal or slightly elevated protein without tumor cells. Laboratory investigations including CSF glucose, Gram stain, and culture help differentiate meningism caused by infectious meningitis from neoplastic processes seen in intracranial tumors.
Treatment Modalities and Management Strategies
Treatment of intracranial tumors primarily involves surgical resection, radiation therapy, and chemotherapy, tailored to tumor type, size, and location, aiming to reduce mass effect and prevent neurological deterioration. Management of meningism focuses on addressing underlying infections or inflammatory causes with antibiotics, antivirals, or corticosteroids, alongside symptomatic relief such as hydration and pain control. Both conditions require multidisciplinary monitoring including neuroimaging, neurological assessments, and supportive care to optimize patient outcomes and prevent complications.
Prognosis and Patient Outcomes
Intracranial tumors often have a more varied prognosis depending on tumor type, size, and location, with malignant tumors typically leading to poorer patient outcomes due to aggressive growth and neurological damage. Meningism, characterized by symptoms such as neck stiffness and photophobia, generally has a better prognosis as it is often caused by benign conditions like viral infections rather than structural brain lesions. Early and accurate differentiation between intracranial tumors and meningism is crucial for optimizing treatment strategies and improving long-term neurological function and survival rates.
Intracranial tumor Infographic
 libterm.com
libterm.com