Cutaneous lymphoma is a rare type of cancer that begins in the lymphocytes found in the skin, often presenting as patches, plaques, or tumors. Early diagnosis and targeted treatment are crucial for managing symptoms and improving outcomes. Discover more about the causes, symptoms, and treatment options in the rest of this article.
Table of Comparison
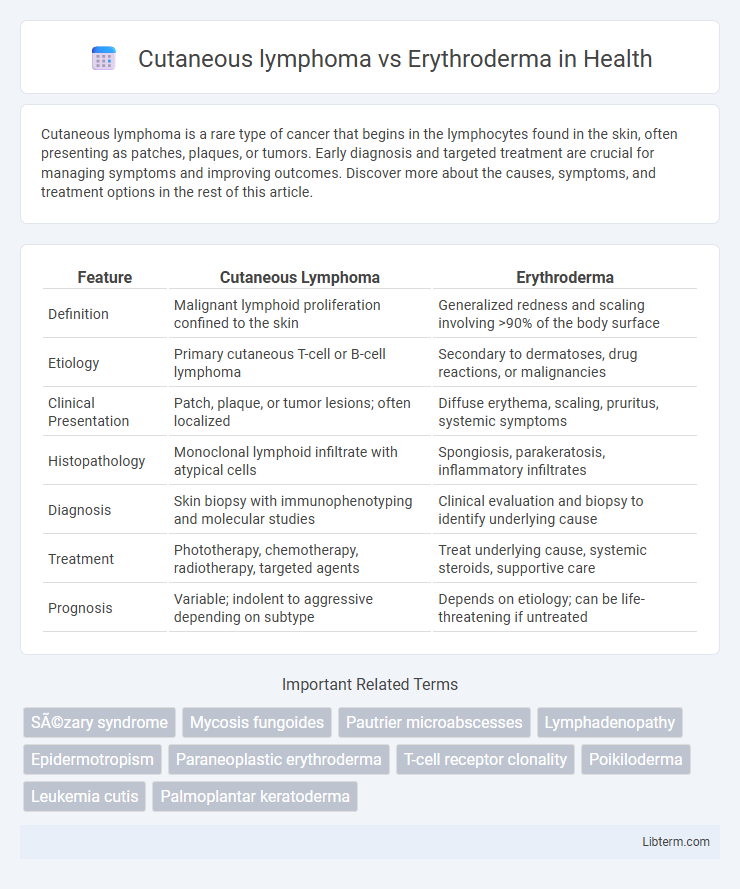
| Feature | Cutaneous Lymphoma | Erythroderma |
|---|---|---|
| Definition | Malignant lymphoid proliferation confined to the skin | Generalized redness and scaling involving >90% of the body surface |
| Etiology | Primary cutaneous T-cell or B-cell lymphoma | Secondary to dermatoses, drug reactions, or malignancies |
| Clinical Presentation | Patch, plaque, or tumor lesions; often localized | Diffuse erythema, scaling, pruritus, systemic symptoms |
| Histopathology | Monoclonal lymphoid infiltrate with atypical cells | Spongiosis, parakeratosis, inflammatory infiltrates |
| Diagnosis | Skin biopsy with immunophenotyping and molecular studies | Clinical evaluation and biopsy to identify underlying cause |
| Treatment | Phototherapy, chemotherapy, radiotherapy, targeted agents | Treat underlying cause, systemic steroids, supportive care |
| Prognosis | Variable; indolent to aggressive depending on subtype | Depends on etiology; can be life-threatening if untreated |
Introduction to Cutaneous Lymphoma and Erythroderma
Cutaneous lymphoma is a rare type of non-Hodgkin lymphoma that primarily affects the skin, presenting with patches, plaques, or tumors due to malignant T-cell or B-cell proliferation. Erythroderma, also known as exfoliative dermatitis, is characterized by widespread redness and scaling involving more than 90% of the body surface, often resulting from underlying dermatologic or systemic conditions. Differentiating between cutaneous lymphoma and erythroderma relies on histopathological analysis and clinical presentation, as both can exhibit extensive skin involvement with significant morbidity.
Definition and Overview
Cutaneous lymphoma is a type of non-Hodgkin lymphoma that primarily affects the skin, characterized by malignant T-cells or B-cells infiltrating the epidermis and dermis, leading to patches, plaques, or tumors. Erythroderma, also known as exfoliative dermatitis, is a severe inflammatory skin condition marked by widespread redness, scaling, and shedding involving more than 90% of the body surface area, often resulting from underlying diseases such as psoriasis, drug reactions, or cutaneous lymphoma itself. Differentiating cutaneous lymphoma from erythroderma is crucial, as cutaneous lymphoma is a malignancy requiring oncologic management, whereas erythroderma is a dermatologic emergency that demands prompt supportive care and treatment of its underlying cause.
Epidemiology and Risk Factors
Cutaneous lymphoma, primarily mycosis fungoides, typically affects adults aged 50-60 with a slight male predominance, often linked to chronic immune dysregulation and genetic predisposition. Erythroderma, a severe inflammatory skin condition, has a broader age distribution and is commonly triggered by pre-existing dermatoses, drug reactions, or malignancies, including cutaneous lymphomas. Epidemiological data highlight that cutaneous lymphoma represents a rare subset of non-Hodgkin lymphomas, whereas erythroderma's incidence correlates with underlying systemic diseases and environmental exposures.
Pathophysiology: Cutaneous Lymphoma vs Erythroderma
Cutaneous lymphoma arises from malignant clonal T-cell or B-cell proliferation localized in the skin, leading to infiltration and disruption of normal epidermal and dermal architecture. Erythroderma, a severe inflammatory condition, involves widespread erythema and scaling caused by diverse etiologies such as psoriasis, drug reactions, or underlying malignancies, driven by immune dysregulation and epidermal hyperplasia. The pathophysiology of cutaneous lymphoma centers on neoplastic immune cell expansion, whereas erythroderma results from extensive cutaneous inflammation and barrier dysfunction.
Clinical Features and Presentation
Cutaneous lymphoma commonly presents as persistent, scaly patches or plaques with varying erythema and may progress to tumors or ulcerations, often accompanied by pruritus and lymphadenopathy. Erythroderma features widespread erythema covering more than 90% of the body surface area, intense scaling, and diffuse skin desquamation, frequently associated with systemic symptoms like fever and malaise. Differentiating the two relies on the chronicity, lesion morphology, and histopathological examination revealing malignant T-cell infiltrates in cutaneous lymphoma versus inflammatory infiltrates in erythroderma.
Diagnostic Criteria and Procedures
Cutaneous lymphoma diagnosis relies on skin biopsy with histopathological examination revealing atypical lymphocytes, immunophenotyping showing clonal T-cell populations, and molecular studies such as T-cell receptor gene rearrangement. Erythroderma diagnosis focuses on clinical assessment indicating widespread erythema and scaling, supported by skin biopsy to rule out malignancy and detect underlying dermatoses, alongside laboratory tests including complete blood count and serum IgE levels. Differentiating these conditions requires integrating clinical presentation, histology, immunohistochemistry, and molecular diagnostics to identify lymphoma-specific markers versus inflammatory or reactive skin changes.
Histopathological Differences
Cutaneous lymphoma histopathology reveals atypical lymphoid infiltrates with epidermotropism and Pautrier microabscesses, whereas erythroderma typically shows a dense, mixed inflammatory infiltrate without clonal lymphocyte proliferation. Immunohistochemistry in cutaneous lymphoma often demonstrates monoclonal T-cell populations, contrasting with the polyclonal inflammatory cells seen in erythroderma biopsies. Epidermal changes such as spongiosis and parakeratosis are prominent in erythroderma but less characteristic of cutaneous lymphoma.
Treatment Options and Management
Cutaneous lymphoma treatment often involves targeted therapies such as phototherapy, topical corticosteroids, systemic retinoids, or chemotherapy depending on the lymphoma subtype and stage. Management of erythroderma requires addressing the underlying cause, which may include systemic corticosteroids, immunosuppressive agents, or biologic therapies for inflammatory or neoplastic etiology. Both conditions necessitate close monitoring to prevent complications like secondary infections and organ dysfunction during treatment.
Prognosis and Outcomes
Cutaneous lymphoma generally carries a variable prognosis depending on the subtype, with mycosis fungoides often demonstrating indolent progression and potential long-term survival, whereas Sezary syndrome is associated with poorer outcomes due to aggressive disease behavior and systemic involvement. Erythroderma prognosis depends largely on the underlying etiology; idiopathic or secondary erythroderma from infections or drug reactions often resolves with treatment, while erythroderma caused by cutaneous lymphoma or psoriasis may lead to chronic morbidity and increased mortality risk. Early diagnosis and targeted therapy significantly influence outcomes in both conditions, emphasizing the importance of accurate differentiation for optimal patient management.
Key Differences and Summary
Cutaneous lymphoma is a type of non-Hodgkin lymphoma that primarily affects the skin, characterized by malignant T-cells or B-cells infiltrating the epidermis and dermis, often presenting as patches, plaques, or tumors. Erythroderma, also known as exfoliative dermatitis, involves widespread redness and scaling of more than 90% of the body surface, typically resulting from inflammatory skin diseases, drug reactions, or malignancies, but is not a cancer itself. Differentiating them relies on histopathological examination, clinical presentation, immunophenotyping, and patient history, with cutaneous lymphoma requiring targeted oncologic treatment while erythroderma management focuses on controlling inflammation and identifying underlying causes.
Cutaneous lymphoma Infographic
 libterm.com
libterm.com