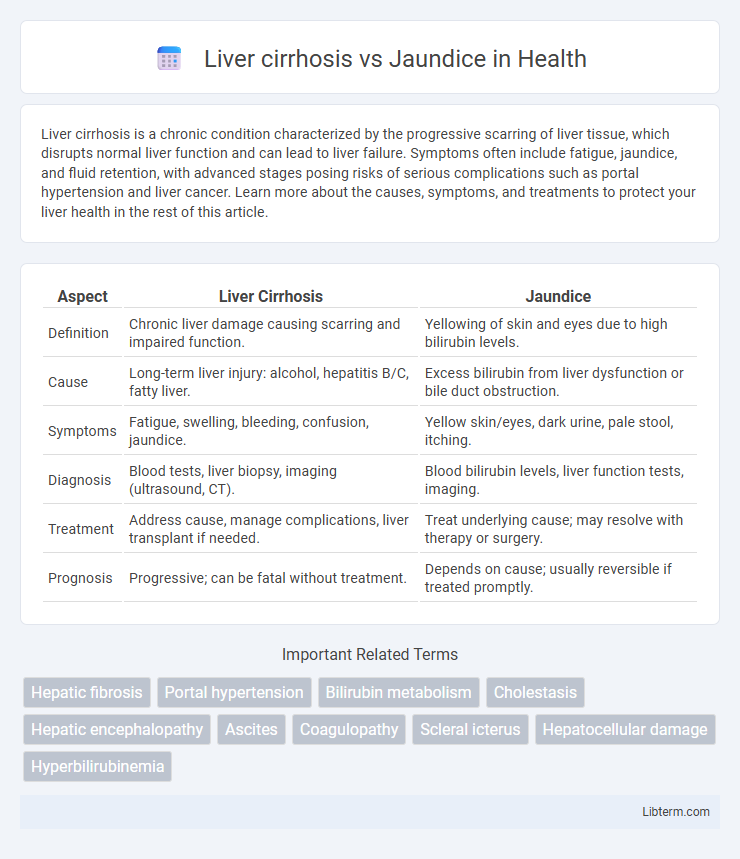
Liver cirrhosis is a chronic condition characterized by the progressive scarring of liver tissue, which disrupts normal liver function and can lead to liver failure. Symptoms often include fatigue, jaundice, and fluid retention, with advanced stages posing risks of serious complications such as portal hypertension and liver cancer. Learn more about the causes, symptoms, and treatments to protect your liver health in the rest of this article.
Table of Comparison
| Aspect | Liver Cirrhosis | Jaundice |
|---|---|---|
| Definition | Chronic liver damage causing scarring and impaired function. | Yellowing of skin and eyes due to high bilirubin levels. |
| Cause | Long-term liver injury: alcohol, hepatitis B/C, fatty liver. | Excess bilirubin from liver dysfunction or bile duct obstruction. |
| Symptoms | Fatigue, swelling, bleeding, confusion, jaundice. | Yellow skin/eyes, dark urine, pale stool, itching. |
| Diagnosis | Blood tests, liver biopsy, imaging (ultrasound, CT). | Blood bilirubin levels, liver function tests, imaging. |
| Treatment | Address cause, manage complications, liver transplant if needed. | Treat underlying cause; may resolve with therapy or surgery. |
| Prognosis | Progressive; can be fatal without treatment. | Depends on cause; usually reversible if treated promptly. |
Understanding Liver Cirrhosis: Definition and Causes
Liver cirrhosis is a chronic liver disease characterized by irreversible scarring and impaired liver function due to long-term damage. Common causes include chronic alcohol abuse, hepatitis B and C infections, non-alcoholic fatty liver disease (NAFLD), and autoimmune hepatitis. Unlike jaundice, which is a symptom defined by yellowing of the skin and eyes due to elevated bilirubin levels, cirrhosis is an underlying condition leading to liver failure and may cause jaundice as a complication.
What is Jaundice? Key Facts and Triggers
Jaundice is a medical condition characterized by the yellowing of the skin and eyes caused by elevated levels of bilirubin in the blood, often signaling underlying liver dysfunction. Key facts about jaundice include its role as a symptom rather than a disease itself, with common triggers such as liver cirrhosis, hepatitis, gallstones, and hemolytic anemia. Identifying the root cause is essential for appropriate treatment, as jaundice indicates impaired liver processing or bile flow obstruction.
How Liver Cirrhosis and Jaundice Are Related
Liver cirrhosis is a chronic condition characterized by irreversible scarring and impaired liver function, often leading to the accumulation of bilirubin, a yellow pigment responsible for jaundice. Jaundice manifests as yellowing of the skin and eyes due to elevated bilirubin levels, commonly occurring as a direct consequence of liver cirrhosis. The relationship between liver cirrhosis and jaundice lies in the liver's diminished ability to process and excrete bilirubin, making jaundice a key symptom of advanced cirrhosis.
Major Causes: Liver Cirrhosis vs Jaundice
Liver cirrhosis primarily results from chronic alcohol abuse, hepatitis B and C infections, and non-alcoholic fatty liver disease (NAFLD), leading to irreversible liver scarring and impaired function. Jaundice, characterized by yellowing of the skin and eyes, arises due to elevated bilirubin levels caused by liver diseases, bile duct obstruction, hemolytic anemia, or genetic disorders like Gilbert's syndrome. Understanding these distinct etiologies is crucial for accurate diagnosis and targeted treatment of each condition.
Symptoms of Liver Cirrhosis Compared to Jaundice
Liver cirrhosis symptoms include fatigue, easy bruising, swelling in the legs and abdomen, and jaundice, which manifests as yellowing of the skin and eyes. Jaundice primarily presents with yellowing due to elevated bilirubin levels but lacks the systemic complications such as portal hypertension and liver dysfunction seen in cirrhosis. Unlike jaundice alone, liver cirrhosis leads to symptoms like itching, confusion from hepatic encephalopathy, and dark urine, reflecting widespread liver damage.
Diagnostic Methods for Cirrhosis and Jaundice
Liver cirrhosis is primarily diagnosed through liver biopsy, elastography, and imaging techniques such as ultrasound, CT scan, and MRI to assess fibrosis and liver structure changes. Jaundice diagnosis involves evaluating serum bilirubin levels, liver function tests (LFTs), and imaging studies like ultrasound or MRCP to identify bile duct obstruction or hemolysis causes. Both conditions require careful interpretation of diagnostic findings to differentiate underlying liver dysfunction from biliary obstruction or hemolytic processes.
Complications: Cirrhosis versus Jaundice
Liver cirrhosis complications include portal hypertension, ascites, hepatic encephalopathy, and increased risk of hepatocellular carcinoma due to chronic liver damage. Jaundice itself is a symptom characterized by elevated bilirubin causing yellowing of the skin and eyes, with complications dependent on the underlying cause, such as hemolysis, bile duct obstruction, or liver dysfunction. Cirrhosis represents a progressive liver pathology with systemic consequences, whereas jaundice is a clinical sign that may indicate various hepatic or hematologic conditions.
Treatment Options: Managing Cirrhosis and Jaundice
Treatment options for liver cirrhosis focus on slowing disease progression and managing complications through medications like diuretics, beta-blockers, or lactulose, alongside lifestyle changes such as alcohol cessation and nutritional support. Jaundice treatment centers on addressing the underlying cause, whether it is liver dysfunction, bile duct obstruction, or hemolytic anemia, with interventions ranging from antiviral therapy for hepatitis to surgical bile duct clearance. Monitoring liver function tests and considering liver transplantation are critical steps in advanced cirrhosis management.
Prevention Strategies: Liver Health and Risk Reduction
Preventing liver cirrhosis involves managing risk factors such as chronic alcohol consumption, viral hepatitis infections (especially hepatitis B and C), and fatty liver disease through vaccination, safe practices, and a balanced diet. Jaundice prevention centers on maintaining healthy liver function and promptly treating underlying liver conditions to avoid bilirubin buildup. Regular medical screenings, avoiding toxins, and adopting liver-friendly lifestyles significantly reduce the risk of liver damage leading to cirrhosis or jaundice.
Prognosis and Outlook: Cirrhosis vs Jaundice
Liver cirrhosis is a progressive, irreversible condition characterized by extensive liver scarring, often leading to complications such as liver failure, portal hypertension, and increased risk of hepatocellular carcinoma, with a generally poor prognosis without liver transplantation. Jaundice, on the other hand, is a symptom of yellowing skin and eyes caused by elevated bilirubin levels, which may result from various reversible conditions like hemolysis, hepatitis, or bile duct obstruction, often having a much better prognosis depending on the underlying cause. The outlook for cirrhosis is typically more severe and chronic, whereas jaundice prognosis varies widely and improves with appropriate treatment of the primary disease.
Liver cirrhosis Infographic
 libterm.com
libterm.com