Hypocalcemia occurs when blood calcium levels drop below normal, leading to symptoms like muscle cramps, tingling, and fatigue. Causes range from vitamin D deficiency and hypoparathyroidism to kidney disease and certain medications. Discover the key signs, causes, and treatments for hypocalcemia by reading the rest of the article.
Table of Comparison
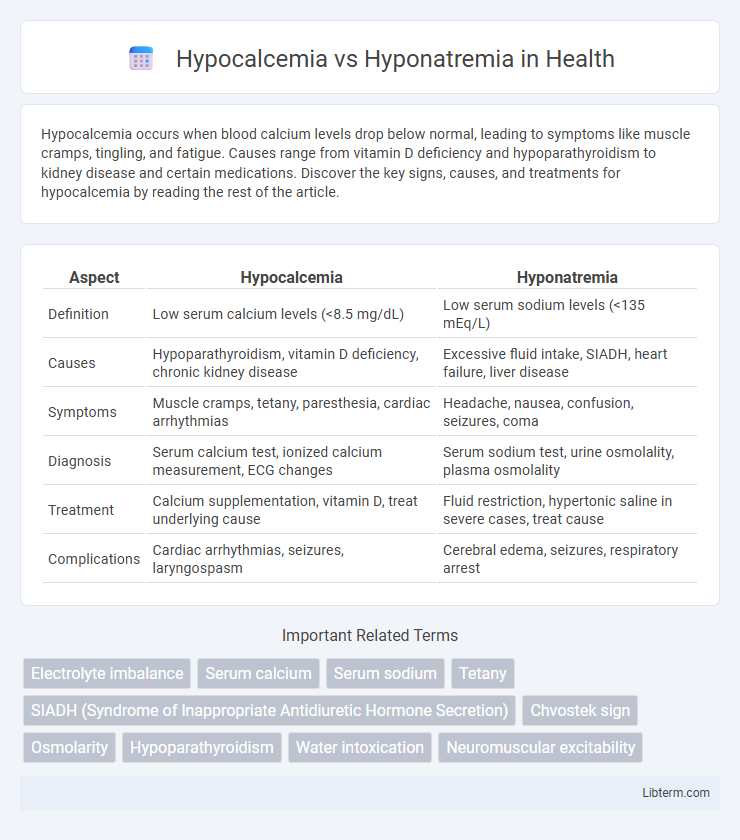
| Aspect | Hypocalcemia | Hyponatremia |
|---|---|---|
| Definition | Low serum calcium levels (<8.5 mg/dL) | Low serum sodium levels (<135 mEq/L) |
| Causes | Hypoparathyroidism, vitamin D deficiency, chronic kidney disease | Excessive fluid intake, SIADH, heart failure, liver disease |
| Symptoms | Muscle cramps, tetany, paresthesia, cardiac arrhythmias | Headache, nausea, confusion, seizures, coma |
| Diagnosis | Serum calcium test, ionized calcium measurement, ECG changes | Serum sodium test, urine osmolality, plasma osmolality |
| Treatment | Calcium supplementation, vitamin D, treat underlying cause | Fluid restriction, hypertonic saline in severe cases, treat cause |
| Complications | Cardiac arrhythmias, seizures, laryngospasm | Cerebral edema, seizures, respiratory arrest |
Understanding Hypocalcemia and Hyponatremia
Hypocalcemia refers to low calcium levels in the blood, which is critical for muscle function, nerve signaling, and bone health, often caused by vitamin D deficiency, parathyroid disorders, or kidney disease. Hyponatremia involves a reduced concentration of sodium in the blood, disrupting cellular function and fluid balance, frequently resulting from excessive fluid intake, heart failure, or certain medications. Both conditions require precise diagnosis and targeted treatment to restore electrolyte balance and prevent severe complications such as seizures or cardiac arrhythmias.
Key Differences in Electrolyte Imbalances
Hypocalcemia is characterized by low serum calcium levels below 8.5 mg/dL, primarily affecting neuromuscular function and leading to symptoms such as muscle cramps and tetany. Hyponatremia involves decreased sodium concentration under 135 mEq/L, causing cellular swelling and neurological symptoms like confusion and seizures. The fundamental difference lies in calcium regulating muscle contraction and nerve signaling, while sodium controls fluid balance and nerve impulse transmission.
Causes of Hypocalcemia
Hypocalcemia is primarily caused by hypoparathyroidism, vitamin D deficiency, chronic kidney disease, and acute pancreatitis. In contrast, hyponatremia results from factors such as excessive fluid intake, heart failure, or syndrome of inappropriate antidiuretic hormone secretion (SIADH). Understanding the etiology of hypocalcemia involves recognizing disruptions in calcium regulation due to impaired parathyroid hormone secretion or vitamin D metabolism.
Causes of Hyponatremia
Hyponatremia occurs due to excessive water retention or sodium loss, commonly caused by conditions such as heart failure, kidney disease, liver cirrhosis, syndrome of inappropriate antidiuretic hormone secretion (SIADH), and use of diuretics. Other factors contributing to hyponatremia include adrenal insufficiency, hypothyroidism, and excessive water intake leading to dilutional hyponatremia. Understanding these causes is crucial for distinguishing hyponatremia from hypocalcemia, which primarily involves calcium imbalance rather than sodium abnormalities.
Signs and Symptoms: Hypocalcemia vs Hyponatremia
Hypocalcemia often presents with neuromuscular irritability signs such as tetany, muscle cramps, paresthesias, and Chvostek's or Trousseau's signs. Hyponatremia primarily manifests through neurological symptoms including headache, nausea, confusion, seizures, and in severe cases, coma due to cerebral edema. Differentiating these electrolyte imbalances clinically relies on recognizing hypocalcemia's characteristic muscle excitability versus hyponatremia's central nervous system disturbances.
Diagnostic Approaches for Each Condition
Diagnostic approaches for hypocalcemia primarily involve serum calcium measurement, ionized calcium levels assessment, and evaluation of parathyroid hormone (PTH) and vitamin D status to determine underlying causes. For hyponatremia, diagnostic strategies emphasize serum sodium concentration analysis, plasma osmolality, and urine osmolality to differentiate between hypovolemic, euvolemic, or hypervolemic states. Both conditions require a thorough clinical history and assessment of renal function to guide targeted treatment and rule out contributing factors.
Treatment Strategies and Management
Treatment of hypocalcemia primarily involves calcium supplementation, either orally or intravenously, alongside vitamin D to enhance calcium absorption and correct underlying deficiencies. Management of hyponatremia includes careful fluid restriction, administration of hypertonic saline in severe cases, and addressing the root causes such as medications or endocrine disorders. Both conditions require close monitoring of electrolyte levels and adjustment of therapy to prevent complications like cardiac arrhythmias in hypocalcemia and cerebral edema in hyponatremia.
Complications and Prognosis
Hypocalcemia can lead to complications such as tetany, cardiac arrhythmias, and seizures, significantly impacting neuromuscular and cardiovascular function. Hyponatremia increases the risk of cerebral edema, seizures, and respiratory arrest due to hypoosmolarity-induced brain swelling. Prognosis depends on severity and rapid correction; untreated hypocalcemia can cause prolonged neuromuscular deficits, while rapid correction of hyponatremia may result in osmotic demyelination syndrome.
Prevention of Electrolyte Disorders
Preventing hypocalcemia involves ensuring adequate dietary intake of calcium and vitamin D, along with regular monitoring in high-risk populations such as post-surgical patients and those with chronic kidney disease. Hyponatremia prevention focuses on managing fluid balance through controlled sodium intake and avoiding excessive free water consumption, especially in patients with heart failure, liver cirrhosis, or syndrome of inappropriate antidiuretic hormone secretion (SIADH). Regular electrolyte monitoring and patient education on symptom recognition remain critical strategies to minimize the risk of both disorders.
When to Seek Medical Attention
Seek medical attention for hypocalcemia if experiencing severe muscle cramps, spasms, numbness, or tingling in the lips and fingers, as these symptoms may indicate dangerously low calcium levels. For hyponatremia, urgent care is necessary when symptoms include confusion, seizures, headache, and severe nausea, signaling critical sodium imbalance. Prompt diagnosis and treatment prevent complications such as cardiac arrhythmias in hypocalcemia and cerebral edema in hyponatremia.
Hypocalcemia Infographic
 libterm.com
libterm.com