Narcolepsy and sleep apnea are distinct sleep disorders that significantly impact your quality of rest and daytime alertness. While narcolepsy causes sudden sleep attacks and excessive daytime sleepiness, sleep apnea results in interrupted breathing patterns leading to fragmented sleep and fatigue. Explore the full article to understand the symptoms, diagnosis, and effective treatments for these conditions.
Table of Comparison
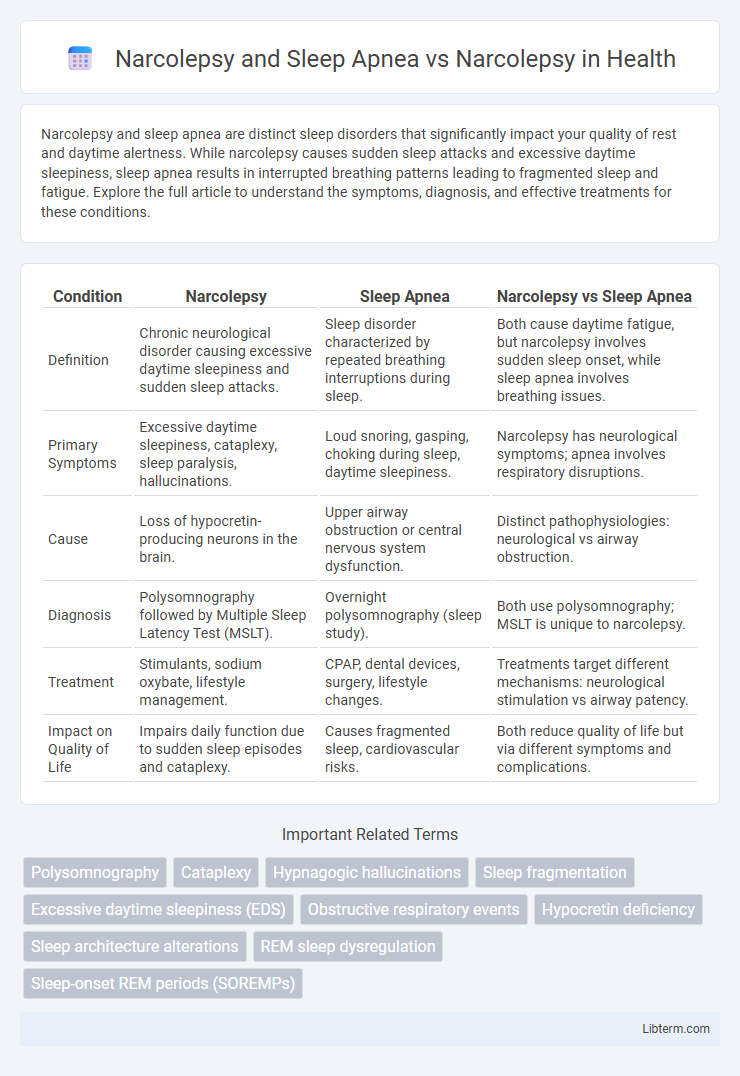
| Condition | Narcolepsy | Sleep Apnea | Narcolepsy vs Sleep Apnea |
|---|---|---|---|
| Definition | Chronic neurological disorder causing excessive daytime sleepiness and sudden sleep attacks. | Sleep disorder characterized by repeated breathing interruptions during sleep. | Both cause daytime fatigue, but narcolepsy involves sudden sleep onset, while sleep apnea involves breathing issues. |
| Primary Symptoms | Excessive daytime sleepiness, cataplexy, sleep paralysis, hallucinations. | Loud snoring, gasping, choking during sleep, daytime sleepiness. | Narcolepsy has neurological symptoms; apnea involves respiratory disruptions. |
| Cause | Loss of hypocretin-producing neurons in the brain. | Upper airway obstruction or central nervous system dysfunction. | Distinct pathophysiologies: neurological vs airway obstruction. |
| Diagnosis | Polysomnography followed by Multiple Sleep Latency Test (MSLT). | Overnight polysomnography (sleep study). | Both use polysomnography; MSLT is unique to narcolepsy. |
| Treatment | Stimulants, sodium oxybate, lifestyle management. | CPAP, dental devices, surgery, lifestyle changes. | Treatments target different mechanisms: neurological stimulation vs airway patency. |
| Impact on Quality of Life | Impairs daily function due to sudden sleep episodes and cataplexy. | Causes fragmented sleep, cardiovascular risks. | Both reduce quality of life but via different symptoms and complications. |
Understanding Narcolepsy: Key Symptoms and Causes
Narcolepsy is a chronic neurological disorder characterized by excessive daytime sleepiness, sudden muscle weakness (cataplexy), hallucinations, and sleep paralysis due to the brain's inability to regulate sleep-wake cycles. Sleep apnea, unlike narcolepsy, involves repeated interruptions in breathing during sleep, leading to fragmented rest and daytime fatigue but not the sudden sleep attacks seen in narcolepsy. Understanding narcolepsy's key symptoms and causes, including genetic factors and the loss of hypocretin-producing neurons, is essential for distinguishing it from sleep apnea and ensuring accurate diagnosis and treatment.
What Is Sleep Apnea? Types and Major Risk Factors
Sleep apnea is a sleep disorder characterized by repeated interruptions in breathing during sleep, leading to fragmented sleep and reduced oxygen levels. The main types of sleep apnea include obstructive sleep apnea (OSA), caused by physical blockage of the airway; central sleep apnea (CSA), resulting from the brain's failure to send proper signals to muscles controlling breathing; and complex sleep apnea syndrome, a combination of both OSA and CSA. Major risk factors for sleep apnea include obesity, age over 40, male gender, family history, smoking, and anatomical features like a thick neck or narrow airway.
Narcolepsy vs Sleep Apnea: Overlapping and Unique Symptoms
Narcolepsy and sleep apnea both cause excessive daytime sleepiness, but narcolepsy uniquely includes sudden muscle weakness (cataplexy) and sleep paralysis, which are absent in sleep apnea. Sleep apnea features disrupted breathing during sleep leading to frequent awakenings, while narcolepsy involves abnormal REM sleep regulation. Overlapping symptoms such as fatigue and cognitive impairment often lead to diagnostic confusion, necessitating polysomnography and multiple sleep latency testing for accurate differentiation.
Diagnosis: Differentiating Narcolepsy from Sleep Apnea
Diagnosis of narcolepsy involves polysomnography followed by a Multiple Sleep Latency Test (MSLT), distinguishing it from sleep apnea, which is primarily identified through overnight sleep studies measuring breathing disruptions. Narcolepsy is characterized by excessive daytime sleepiness, cataplexy, sleep paralysis, and hypnagogic hallucinations, whereas sleep apnea presents with obstructive breathing events, loud snoring, and frequent awakenings. Accurate differentiation requires evaluating sleep architecture, respiratory patterns, and sleep latency to ensure targeted treatment strategies for each disorder.
Sleep Study Tests: How Narcolepsy and Sleep Apnea Are Detected
Sleep study tests such as polysomnography and multiple sleep latency tests (MSLT) are crucial for distinguishing narcolepsy from sleep apnea by analyzing patterns of sleep stages and breathing irregularities. Polysomnography monitors brain waves, oxygen levels, heart rate, and airflow to detect obstructive sleep apnea, while MSLT measures daytime sleepiness and rapid eye movement (REM) onset to diagnose narcolepsy. Accurate diagnosis through these tests enables tailored treatment plans for managing excessive daytime sleepiness and respiratory disruptions.
Impact of Both Disorders on Daily Life and Functioning
Narcolepsy and sleep apnea both significantly disrupt daily life but affect functioning in distinct ways. Narcolepsy causes excessive daytime sleepiness, sudden sleep attacks, and impaired alertness that hinder concentration, work performance, and safety. Sleep apnea leads to fragmented sleep and oxygen deprivation, resulting in fatigue, cardiovascular risks, and diminished cognitive function, which also compromise quality of life and productivity.
Treatment Options: Narcolepsy Compared to Sleep Apnea
Narcolepsy treatment primarily involves stimulant medications such as modafinil and sodium oxybate to manage excessive daytime sleepiness and cataplexy, while behavioral strategies like scheduled naps complement pharmacological approaches. In contrast, sleep apnea relies heavily on continuous positive airway pressure (CPAP) therapy to maintain airway patency during sleep, alongside lifestyle modifications including weight loss and positional therapy. Unlike apnea, narcolepsy treatment does not focus on respiratory interventions but targets neurochemical imbalances affecting sleep-wake regulation.
Can Narcolepsy and Sleep Apnea Occur Together?
Narcolepsy and sleep apnea can occur together, complicating diagnosis and treatment due to overlapping symptoms like excessive daytime sleepiness. Sleep apnea, characterized by repeated airway obstruction during sleep, may exacerbate the fatigue experienced by narcolepsy patients, who suffer from sudden sleep attacks and disrupted REM sleep. Comprehensive sleep studies, including polysomnography, are essential to differentiate and manage both conditions effectively.
Living with Narcolepsy and/or Sleep Apnea: Coping Strategies
Living with narcolepsy requires consistent sleep schedules and strategic short naps to manage excessive daytime sleepiness, while sleep apnea demands adherence to CPAP therapy to ensure airway patency during sleep. Combining behavioral modifications like avoiding alcohol and practicing good sleep hygiene benefits individuals with both conditions, mitigating symptoms and improving quality of life. Regular medical monitoring and support groups enhance coping strategies, promoting better symptom control and mental health.
Seeking Professional Help: When to Consult a Sleep Specialist
Consult a sleep specialist if experiencing excessive daytime sleepiness, sudden muscle weakness, or frequent nighttime awakenings, as these symptoms may indicate narcolepsy or sleep apnea. Accurate diagnosis requires comprehensive sleep studies and expert evaluation to differentiate between the two conditions. Timely professional intervention improves management strategies, reduces complications, and enhances quality of life for individuals with narcolepsy or sleep apnea.
Narcolepsy and Sleep Apnea Infographic
 libterm.com
libterm.com