Spirometry and lung volume measurement are essential diagnostic tools for assessing respiratory health and detecting conditions like asthma, COPD, and restrictive lung diseases. Accurate measurement of lung volumes and airflow helps tailor treatment plans to improve Your breathing efficiency and overall lung function. Explore the rest of the article to understand how these tests provide vital insights into your respiratory system.
Table of Comparison
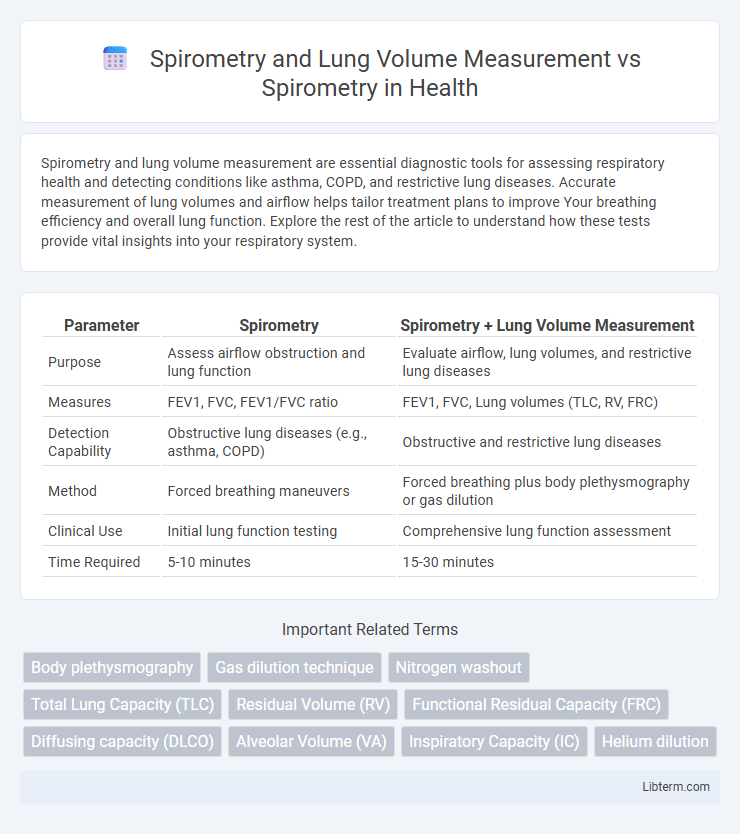
| Parameter | Spirometry | Spirometry + Lung Volume Measurement |
|---|---|---|
| Purpose | Assess airflow obstruction and lung function | Evaluate airflow, lung volumes, and restrictive lung diseases |
| Measures | FEV1, FVC, FEV1/FVC ratio | FEV1, FVC, Lung volumes (TLC, RV, FRC) |
| Detection Capability | Obstructive lung diseases (e.g., asthma, COPD) | Obstructive and restrictive lung diseases |
| Method | Forced breathing maneuvers | Forced breathing plus body plethysmography or gas dilution |
| Clinical Use | Initial lung function testing | Comprehensive lung function assessment |
| Time Required | 5-10 minutes | 15-30 minutes |
Introduction to Pulmonary Function Testing
Pulmonary function testing encompasses spirometry and lung volume measurement, both critical for evaluating respiratory health. Spirometry measures airflow and volume during forced breathing maneuvers, aiding in the diagnosis of obstructive and restrictive lung diseases. Lung volume measurement quantifies total lung capacity and residual volume, providing comprehensive insight into lung mechanics and detecting conditions that spirometry alone might miss.
Overview of Spirometry
Spirometry is a fundamental pulmonary function test that measures the volume and flow of air during inhalation and exhalation, providing critical data on lung capacity and airflow obstruction. It assesses parameters such as Forced Vital Capacity (FVC) and Forced Expiratory Volume in one second (FEV1), essential for diagnosing conditions like asthma and chronic obstructive pulmonary disease (COPD). Unlike comprehensive lung volume measurement, which quantifies total lung capacity and residual volume, spirometry primarily focuses on dynamic airflow and volume changes during forced breathing maneuvers.
Fundamentals of Lung Volume Measurement
Spirometry primarily measures airflow and volume during forced expiration and inspiration, providing key data on lung function such as FEV1 and FVC. Lung volume measurement goes beyond spirometry by quantifying static lung volumes, including total lung capacity (TLC), residual volume (RV), and functional residual capacity (FRC), essential for detecting restrictive lung diseases and air trapping. Techniques like body plethysmography, gas dilution, and nitrogen washout are fundamental methods for accurately assessing these lung volumes when spirometry alone is insufficient.
Key Differences: Spirometry vs. Lung Volume Measurement
Spirometry measures airflow and volume during forced breathing to assess lung function by capturing parameters like FEV1 and FVC, while lung volume measurement quantifies static lung volumes such as total lung capacity (TLC) and residual volume (RV) that cannot be measured by spirometry alone. Spirometry is primarily used to diagnose obstructive and restrictive lung diseases, whereas lung volume measurement provides detailed insight into lung mechanics and gas trapping, essential in complex respiratory diagnoses. Techniques for lung volume measurement include body plethysmography and gas dilution methods, which complement spirometry findings for comprehensive pulmonary evaluation.
Clinical Applications of Spirometry
Spirometry is essential in clinical settings for diagnosing obstructive and restrictive lung diseases by measuring airflow and volume during forced exhalation. Lung volume measurement complements spirometry by providing critical data on total lung capacity, vital capacity, and residual volume, which helps differentiate between various pulmonary disorders. Together, these tests enable precise assessment of respiratory function, guiding treatment decisions in conditions like asthma, COPD, and interstitial lung disease.
Clinical Importance of Lung Volume Measurement
Lung volume measurement provides critical data on total lung capacity, residual volume, and functional residual capacity that spirometry alone cannot assess, enabling precise diagnosis of restrictive lung diseases. Spirometry primarily evaluates airflow limitations by measuring forced expiratory volume and forced vital capacity, but lacks insights into trapped air and lung hyperinflation. Incorporating lung volume measurement enhances clinical decision-making by differentiating between obstructive and restrictive pathologies, optimizing treatment strategies for conditions such as pulmonary fibrosis and chronic obstructive pulmonary disease (COPD).
Limitations of Spirometry Alone
Spirometry alone cannot measure lung volumes such as residual volume, total lung capacity, or functional residual capacity, limiting its ability to fully assess restrictive lung diseases. It primarily evaluates airflow obstruction and cannot distinguish between different causes of reduced lung function without complementary lung volume measurements. Relying solely on spirometry may lead to underdiagnosis or misclassification of complex pulmonary conditions, highlighting the necessity of combined testing for comprehensive respiratory assessment.
Advantages of Comprehensive Lung Volume Assessment
Comprehensive lung volume assessment, combining spirometry and lung volume measurements, provides a more detailed evaluation of pulmonary function, detecting restrictive lung diseases that spirometry alone might miss. It quantifies total lung capacity (TLC) and residual volume (RV), offering insights into airway obstruction and hyperinflation. This integrated approach enhances diagnostic accuracy and guides targeted treatment strategies for conditions such as COPD and interstitial lung disease.
When to Use Spirometry vs. Full Lung Volume Measurement
Spirometry is ideal for initial screening and assessing obstructive lung diseases like asthma and COPD by measuring forced expiratory volumes and flow rates. Full lung volume measurement is necessary when evaluating restrictive lung diseases, complex respiratory conditions, or when spirometry results are inconclusive, as it quantifies total lung capacity, residual volume, and functional residual capacity. Clinicians choose full lung volume tests to obtain detailed pulmonary function data that spirometry alone cannot provide.
Summary: Optimizing Respiratory Evaluation
Spirometry provides essential measurements of airflow and lung function, primarily assessing forced expiratory volume and capacity to diagnose obstructive and restrictive lung diseases. Lung volume measurement complements spirometry by quantifying lung volumes such as total lung capacity (TLC) and residual volume (RV), offering a comprehensive view of lung mechanics and gas exchange capacity. Combining spirometry with lung volume measurement optimizes respiratory evaluation, enabling precise diagnosis, treatment planning, and monitoring of pulmonary conditions.
Spirometry and Lung Volume Measurement Infographic
 libterm.com
libterm.com