Candidiasis is a fungal infection caused by Candida species, commonly affecting the mouth, skin, and genital areas. Symptoms vary depending on the site of infection but often include redness, itching, and discomfort. Learn more about effective treatments and prevention strategies to protect your health.
Table of Comparison
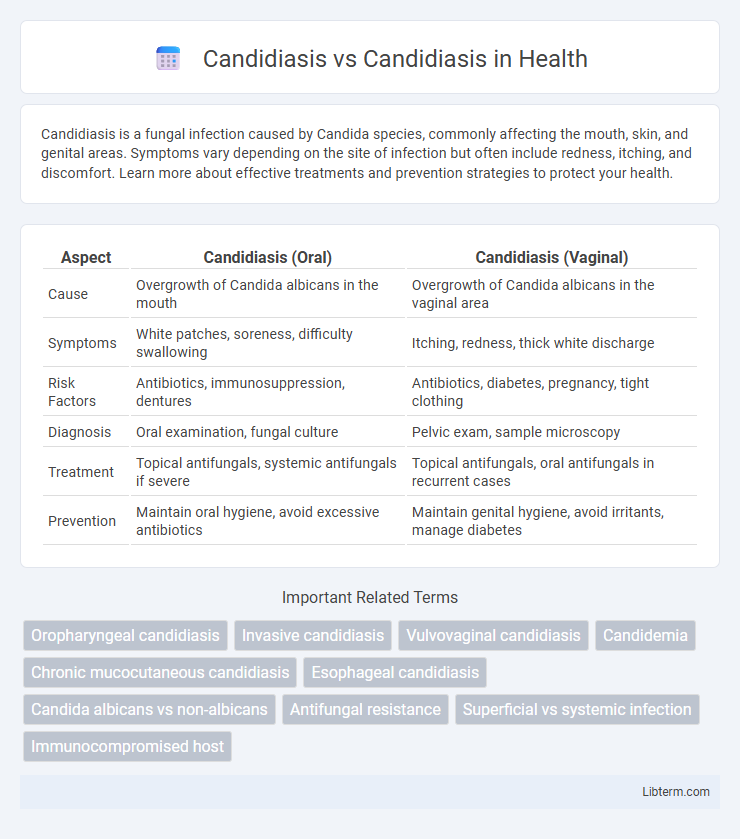
| Aspect | Candidiasis (Oral) | Candidiasis (Vaginal) |
|---|---|---|
| Cause | Overgrowth of Candida albicans in the mouth | Overgrowth of Candida albicans in the vaginal area |
| Symptoms | White patches, soreness, difficulty swallowing | Itching, redness, thick white discharge |
| Risk Factors | Antibiotics, immunosuppression, dentures | Antibiotics, diabetes, pregnancy, tight clothing |
| Diagnosis | Oral examination, fungal culture | Pelvic exam, sample microscopy |
| Treatment | Topical antifungals, systemic antifungals if severe | Topical antifungals, oral antifungals in recurrent cases |
| Prevention | Maintain oral hygiene, avoid excessive antibiotics | Maintain genital hygiene, avoid irritants, manage diabetes |
Understanding Candidiasis: Definition and Overview
Candidiasis is a fungal infection caused by Candida species, primarily Candida albicans, affecting mucous membranes, skin, and sometimes internal organs. This opportunistic infection thrives in warm, moist environments and can lead to conditions such as oral thrush, vaginal yeast infections, and invasive candidiasis in immunocompromised individuals. Recognizing the clinical presentations and risk factors of candidiasis is essential for accurate diagnosis and effective antifungal treatment.
Types of Candidiasis: Oral vs. Genital vs. Invasive
Candidiasis presents in various forms, with oral candidiasis affecting the mouth and throat, characterized by white patches and discomfort, primarily caused by Candida albicans. Genital candidiasis, commonly known as a yeast infection, involves the mucous membranes of the genital area, leading to itching, redness, and discharge, often triggered by hormonal changes or antibiotic use. Invasive candidiasis occurs when Candida enters the bloodstream or internal organs, posing severe risks especially in immunocompromised patients, requiring prompt antifungal treatment to prevent systemic infection.
Causes and Risk Factors of Candidiasis
Candidiasis is caused by an overgrowth of Candida species, primarily Candida albicans, which normally reside in the human body without causing harm. Risk factors for candidiasis include immunosuppression, diabetes mellitus, antibiotic use, hormonal changes such as pregnancy, and medical devices like catheters. Conditions that disrupt the normal microbiota or weaken the immune system significantly increase susceptibility to fungal infections caused by Candida.
Candidiasis Symptoms: How They Differ
Candidiasis primarily presents with symptoms such as white patches on the tongue and inner cheeks, redness, and soreness in the mouth, while vaginal candidiasis typically causes itching, redness, and thick white discharge. Oral candidiasis often leads to difficulty swallowing and a burning sensation, contrasting with the vaginal form, which may result in pain during intercourse and urination. Understanding these distinct symptom patterns helps in accurate diagnosis and effective treatment of the different types of candidiasis.
Diagnostic Methods for Candidiasis
Diagnostic methods for candidiasis primarily include microscopic examination, culture techniques, and molecular assays to identify Candida species accurately. Direct microscopy with potassium hydroxide (KOH) preparation reveals budding yeast cells and pseudohyphae, while culture on Sabouraud dextrose agar facilitates species identification and antifungal susceptibility testing. Polymerase chain reaction (PCR) and other nucleic acid-based tests provide rapid, sensitive detection, essential for differentiating between superficial and invasive candidiasis.
Candidiasis Treatment Options: Similarities and Differences
Candidiasis treatment options primarily involve antifungal medications such as fluconazole, clotrimazole, and nystatin, which are effective across various forms of the infection including oral thrush and vaginal yeast infections. Similarities in treatment include the common use of topical and systemic antifungals, while differences arise in duration, dosage, and administration route tailored to the infection site and severity. Understanding these nuances ensures targeted therapy, minimizing resistance risk and improving patient outcomes.
Prevention Strategies for Various Forms of Candidiasis
Prevention strategies for various forms of candidiasis focus on maintaining good hygiene, reducing moisture in susceptible areas, and managing underlying health conditions such as diabetes or immune deficiencies. Using antifungal prophylaxis in high-risk patients, such as those undergoing chemotherapy or with HIV/AIDS, significantly reduces the incidence of invasive candidiasis. Regular monitoring and prompt treatment of early symptoms prevent progression, while avoiding unnecessary antibiotic or corticosteroid use minimizes disruption of normal microbiota that guard against Candida overgrowth.
Potential Complications of Untreated Candidiasis
Untreated candidiasis can lead to severe complications such as systemic candidiasis, which invades the bloodstream and internal organs, posing a life-threatening risk especially in immunocompromised individuals. Chronic mucocutaneous candidiasis may cause persistent infections resistant to standard therapies, contributing to increased morbidity. Invasive candidiasis complications include endocarditis, osteomyelitis, and abscess formation, requiring prompt medical intervention to prevent long-term damage.
Candidiasis: When to Seek Medical Attention
Persistent symptoms of candidiasis, such as intense itching, redness, or white patches in the mouth or genital area, indicate the need for medical attention to prevent complications. If you experience recurrent infections, fever, or pain that does not improve with over-the-counter treatments, consult a healthcare professional promptly. Early diagnosis and treatment with antifungal medications can effectively manage candidiasis and reduce the risk of severe infection.
Key Takeaways: Comparing and Contrasting Candidiasis
Candidiasis refers to fungal infections caused primarily by Candida species, with common forms including oral thrush, vaginal yeast infections, and invasive candidiasis. Differentiating these types is crucial for tailored treatment: superficial candidiasis typically responds well to topical antifungals, while invasive candidiasis requires systemic therapy due to its severity and risk of bloodstream involvement. Understanding the infection site, Candida species involved, and patient immune status guides effective management and improves outcomes.
Candidiasis Infographic
 libterm.com
libterm.com