Sepsis is a life-threatening condition caused by the body's extreme response to infection, leading to tissue damage, organ failure, and potentially death. Early recognition of symptoms such as fever, rapid heartbeat, and confusion is crucial for timely treatment and improving survival chances. Explore the rest of the article to understand how to identify sepsis, its risk factors, and effective treatment options.
Table of Comparison
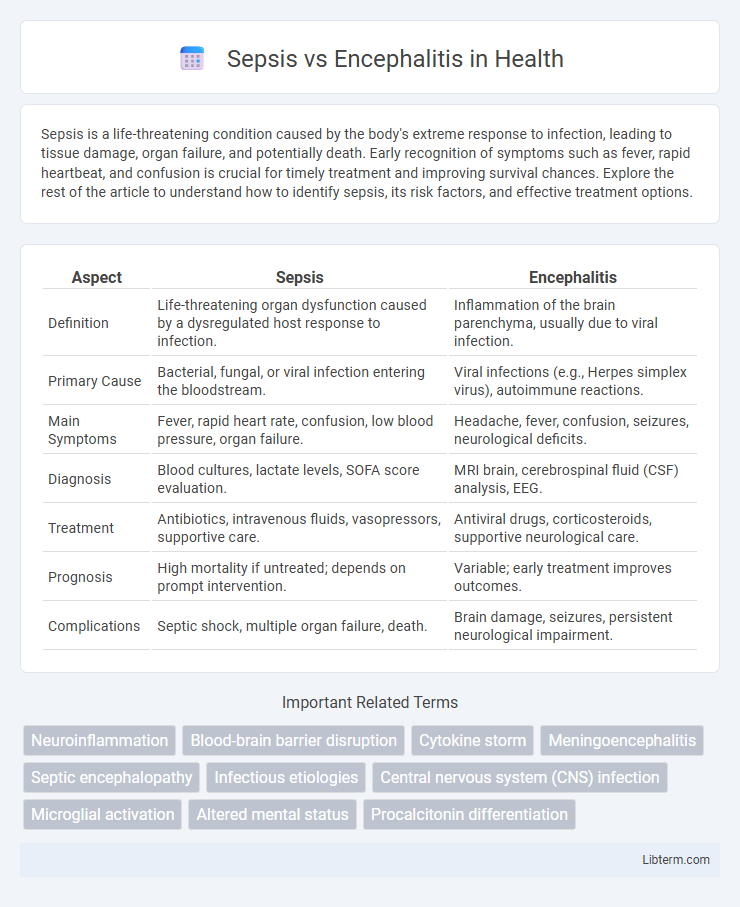
| Aspect | Sepsis | Encephalitis |
|---|---|---|
| Definition | Life-threatening organ dysfunction caused by a dysregulated host response to infection. | Inflammation of the brain parenchyma, usually due to viral infection. |
| Primary Cause | Bacterial, fungal, or viral infection entering the bloodstream. | Viral infections (e.g., Herpes simplex virus), autoimmune reactions. |
| Main Symptoms | Fever, rapid heart rate, confusion, low blood pressure, organ failure. | Headache, fever, confusion, seizures, neurological deficits. |
| Diagnosis | Blood cultures, lactate levels, SOFA score evaluation. | MRI brain, cerebrospinal fluid (CSF) analysis, EEG. |
| Treatment | Antibiotics, intravenous fluids, vasopressors, supportive care. | Antiviral drugs, corticosteroids, supportive neurological care. |
| Prognosis | High mortality if untreated; depends on prompt intervention. | Variable; early treatment improves outcomes. |
| Complications | Septic shock, multiple organ failure, death. | Brain damage, seizures, persistent neurological impairment. |
Introduction to Sepsis and Encephalitis
Sepsis is a life-threatening condition caused by the body's extreme response to infection, leading to tissue damage, organ failure, and potentially death. Encephalitis refers to inflammation of the brain tissue, commonly triggered by viral infections, resulting in symptoms such as headache, fever, confusion, and seizures. Both conditions require prompt medical intervention due to their severe impact on the body and potential neurological complications.
Key Differences Between Sepsis and Encephalitis
Sepsis is a life-threatening systemic inflammatory response caused by infection, leading to widespread organ dysfunction, while encephalitis is an inflammation of the brain tissue typically due to viral infection. Sepsis primarily affects the entire body's organs, resulting in symptoms like fever, rapid heart rate, and hypotension, whereas encephalitis presents neurological symptoms such as confusion, seizures, and altered consciousness. Diagnosis of sepsis relies on blood cultures and markers like lactate levels, whereas encephalitis diagnosis involves cerebrospinal fluid analysis and brain imaging techniques like MRI.
Causes and Risk Factors
Sepsis is primarily caused by a widespread bacterial infection that triggers a systemic inflammatory response, often originating from pneumonia, urinary tract infections, or abdominal infections. Encephalitis results from viral infections such as herpes simplex virus, arboviruses, or autoimmune reactions affecting brain tissue. Risk factors for sepsis include immunosuppression, chronic illnesses, and invasive medical procedures, while encephalitis risk increases with viral exposure, weakened immunity, and geographic location with endemic arboviruses.
Clinical Symptoms Comparison
Sepsis primarily manifests with symptoms such as high fever, rapid heart rate, rapid breathing, confusion, and low blood pressure, reflecting a systemic inflammatory response to infection. Encephalitis presents with neurological symptoms including headache, fever, altered mental status, seizures, and focal neurological deficits, indicating inflammation of the brain tissue. Differentiating clinical features help guide diagnosis, as sepsis affects multiple organs while encephalitis specifically impairs central nervous system function.
Diagnostic Approaches
Diagnostic approaches for sepsis primarily involve blood cultures, complete blood count (CBC), serum lactate levels, and biomarkers such as procalcitonin to detect systemic infection and organ dysfunction. Encephalitis diagnosis relies on neuroimaging techniques like MRI, cerebrospinal fluid (CSF) analysis through lumbar puncture to identify viral or autoimmune causes, and electroencephalography (EEG) to assess brain activity abnormalities. Both conditions require timely laboratory and clinical assessments, but sepsis emphasizes systemic infection markers while encephalitis focuses on central nervous system inflammation indicators.
Laboratory and Imaging Findings
Sepsis typically presents with elevated white blood cell count, increased lactate levels, and positive blood cultures, with imaging often showing signs of source infection such as pneumonia or abscess on chest X-ray or CT scan. Encephalitis is characterized by cerebrospinal fluid (CSF) abnormalities including lymphocytic pleocytosis, elevated protein, and normal or low glucose, with brain MRI revealing hyperintense lesions in the temporal lobes or other affected areas. Distinguishing features include the presence of systemic inflammatory markers in sepsis versus focal neurological abnormalities and CSF changes in encephalitis.
Treatment Strategies for Sepsis vs Encephalitis
Treatment strategies for sepsis prioritize immediate administration of broad-spectrum antibiotics and aggressive fluid resuscitation to stabilize hemodynamics, alongside vasopressors if necessary to maintain blood pressure. Encephalitis treatment often involves antiviral medications, such as acyclovir for herpes simplex virus, combined with supportive care to manage symptoms like seizures or increased intracranial pressure. Early diagnosis and targeted interventions are critical in both conditions to reduce morbidity and improve patient outcomes.
Prognosis and Potential Complications
Sepsis often leads to multi-organ failure and carries a higher mortality rate compared to encephalitis, with long-term complications including chronic fatigue, cognitive impairment, and persistent inflammation. Encephalitis prognosis depends on the causative agent but may result in neurological deficits such as seizures, cognitive dysfunction, and motor impairments. Early diagnosis and treatment are critical in both conditions to reduce the risk of severe complications and improve overall outcomes.
Prevention and Risk Reduction
Preventing sepsis involves prompt treatment of infections, maintaining proper hygiene, and implementing vaccinations against bacteria such as Streptococcus pneumoniae and Neisseria meningitidis. Encephalitis prevention focuses on avoiding mosquito bites in areas endemic to arboviruses, vaccination against viruses like herpes simplex and Japanese encephalitis, and practicing safe hygiene to reduce viral transmission. Risk reduction for both conditions includes managing chronic diseases, early recognition of symptoms, and immediate medical intervention to limit complications.
When to Seek Medical Attention
Seek immediate medical attention if symptoms of sepsis appear, such as high fever, rapid heart rate, difficulty breathing, confusion, or extreme pain, as sepsis can progress rapidly to life-threatening organ failure. Encephalitis requires urgent evaluation when experiencing severe headache, fever, confusion, seizures, or neurological deficits like weakness or speech problems. Early diagnosis and treatment in both conditions are critical to improving outcomes and preventing long-term complications.
Sepsis Infographic
 libterm.com
libterm.com