Rumination involves repetitive and persistent thinking about distressing situations or emotions, which can negatively impact mental health by increasing feelings of anxiety and depression. Understanding the mechanisms behind rumination can help you develop effective coping strategies to reduce its harmful effects. Explore the rest of the article to learn practical tips for managing and overcoming rumination.
Table of Comparison
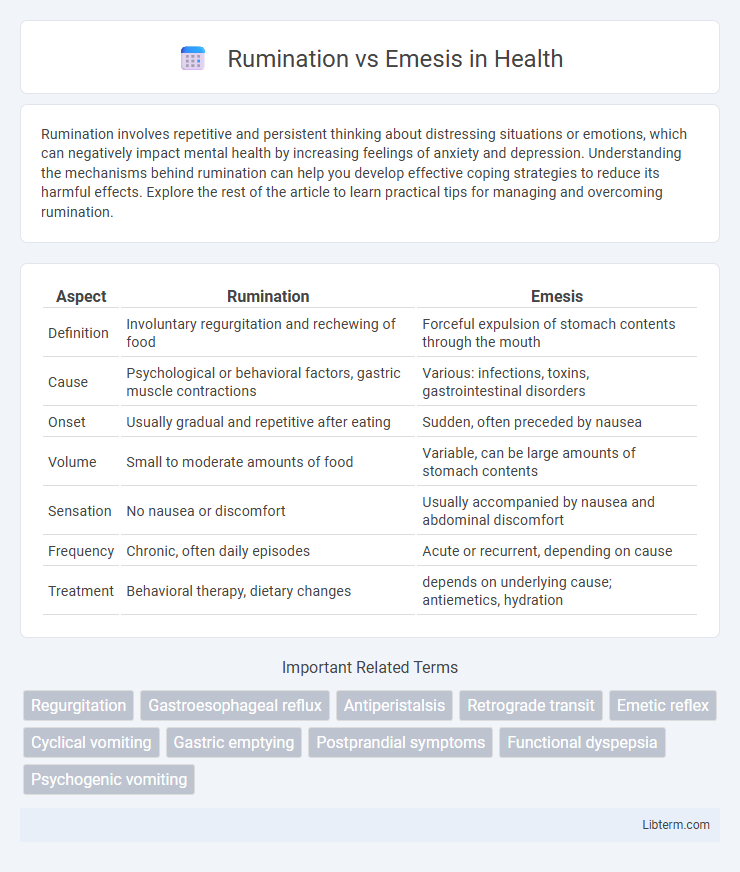
| Aspect | Rumination | Emesis |
|---|---|---|
| Definition | Involuntary regurgitation and rechewing of food | Forceful expulsion of stomach contents through the mouth |
| Cause | Psychological or behavioral factors, gastric muscle contractions | Various: infections, toxins, gastrointestinal disorders |
| Onset | Usually gradual and repetitive after eating | Sudden, often preceded by nausea |
| Volume | Small to moderate amounts of food | Variable, can be large amounts of stomach contents |
| Sensation | No nausea or discomfort | Usually accompanied by nausea and abdominal discomfort |
| Frequency | Chronic, often daily episodes | Acute or recurrent, depending on cause |
| Treatment | Behavioral therapy, dietary changes | depends on underlying cause; antiemetics, hydration |
Understanding Rumination and Emesis
Rumination involves the effortless regurgitation of recently ingested food, which is then rechewed and swallowed or expelled, often linked to behavioral or neurological factors. Emesis, commonly known as vomiting, is a complex reflex typically triggered by gastrointestinal irritation, infections, or central nervous system stimuli, leading to forceful expulsion of stomach contents. Differentiating rumination from emesis is essential for accurate diagnosis and treatment, as rumination is a chronic condition mainly seen in infants and individuals with certain psychological disorders, whereas emesis is an acute protective response to harmful stimuli.
Key Differences Between Rumination and Emesis
Rumination involves the repeated regurgitation and rechewing of previously swallowed food, typically without nausea or vomiting, whereas emesis refers to the forceful expulsion of stomach contents through the mouth, commonly triggered by nausea. Rumination is often a chronic behavioral process linked to disorders such as rumination syndrome, while emesis is usually an acute response to gastrointestinal irritation, infection, or toxins. Key differences include the underlying physiological mechanisms, with rumination resulting from voluntary or involuntary muscle coordination and emesis driven by central nervous system reflexes.
Causes of Rumination: Why It Happens
Rumination occurs primarily due to learned behavioral patterns or underlying psychological stressors that disrupt normal digestive processes. This condition often arises after meals when individuals subconsciously regurgitate and rechew food without nausea or retching, linked to habitual muscle contractions of the esophagus and stomach. Factors such as anxiety, gastroesophageal reflux disease (GERD), and neurogenic disorders contribute to the onset of rumination, distinguishing it from emesis, which is an involuntary reflex triggered by toxins or irritants affecting the brain's vomiting center.
Triggers and Causes of Emesis
Emesis, commonly known as vomiting, is primarily triggered by the activation of the brain's vomiting center in response to stimuli such as gastrointestinal irritation, infections, motion sickness, or central nervous system disorders. Causes of emesis include viral gastroenteritis, food poisoning, migraines, pregnancy (morning sickness), and adverse reactions to medications or toxins. Unlike rumination, which involves effortless regurgitation and re-chewing of food due to behavioral or functional gastrointestinal issues, emesis is an involuntary protective reflex aimed at expelling harmful substances from the stomach.
Symptoms of Rumination Disorder
Rumination disorder is characterized by the repeated regurgitation of food, which is then rechewed, reswallowed, or expelled, without nausea or underlying gastrointestinal issues. Common symptoms include effortless regurgitation occurring within 30 minutes after eating, frequent belching, and the absence of retching or abdominal pain typically associated with emesis. Unlike emesis, which is often forceful and linked to illness, rumination disorder involves a subconscious, habitual behavior that can lead to weight loss and dental erosion if untreated.
Recognizing the Signs of Emesis
Emesis, commonly known as vomiting, is characterized by forceful expulsion of stomach contents through the mouth, often preceded by nausea, retching, and abdominal discomfort. Recognizing the signs of emesis includes observing repeated gagging, excessive salivation, and the presence of bile or partially digested food in vomitus. Differentiating emesis from rumination involves noting the involuntary nature of vomiting versus the voluntary regurgitation and rechewing of food seen in rumination syndrome.
Diagnosis: Rumination vs Emesis
Diagnosis of rumination involves observing effortless, repetitive regurgitation of recently ingested food, usually occurring within minutes of eating and without nausea or retching, while emesis is characterized by forceful expulsion of gastric contents preceded by nausea and abdominal contractions. Diagnostic tools for rumination include patient history, physical examination, and esophageal manometry, whereas emesis diagnosis often requires identifying underlying causes such as gastrointestinal obstruction or infection through imaging and laboratory tests. Differentiating rumination from emesis is crucial for appropriate management, with rumination often linked to behavioral or neurological factors and emesis indicating acute or chronic medical conditions.
Treatment Options for Rumination
Treatment options for rumination primarily involve behavioral therapy, including diaphragmatic breathing exercises to reduce abdominal pressure and prevent regurgitation. In some cases, biofeedback and cognitive-behavioral therapy (CBT) are effective in addressing underlying stress or anxiety contributing to rumination syndrome. Pharmacological treatments are less common but may include medications like baclofen to decrease gastric muscle contractions.
Managing and Treating Emesis
Managing and treating emesis involves identifying underlying causes such as infections, gastrointestinal disorders, or medication side effects to tailor appropriate interventions. Pharmacologic treatments include antiemetics like ondansetron, metoclopramide, and promethazine, which target different pathways to reduce nausea and vomiting. Supportive care with hydration, electrolyte correction, and nutritional support is essential to prevent complications and promote recovery.
Prevention and Long-term Management Strategies
Effective prevention of rumination involves behavioral therapies such as diaphragmatic breathing and habit reversal training to curb regurgitation episodes, while dietary modifications that avoid large, high-fat meals can reduce emesis risk by minimizing gastric irritation. Long-term management of rumination requires consistent psychological support and monitoring to prevent recurrence, whereas chronic emesis often demands medical evaluation to address underlying causes like GERD or gastroparesis, with pharmacologic treatments including antiemetics and prokinetics playing key roles. Both conditions benefit from patient education on symptom recognition and lifestyle adjustments to maintain gastrointestinal health and improve quality of life.
Rumination Infographic
 libterm.com
libterm.com