Bradycardia is a condition characterized by an abnormally slow heart rate, typically fewer than 60 beats per minute, which can lead to fatigue, dizziness, and fainting. Understanding the underlying causes, such as heart block or medication effects, is essential for proper diagnosis and management. Explore the full article to learn how you can recognize symptoms and explore effective treatment options for bradycardia.
Table of Comparison
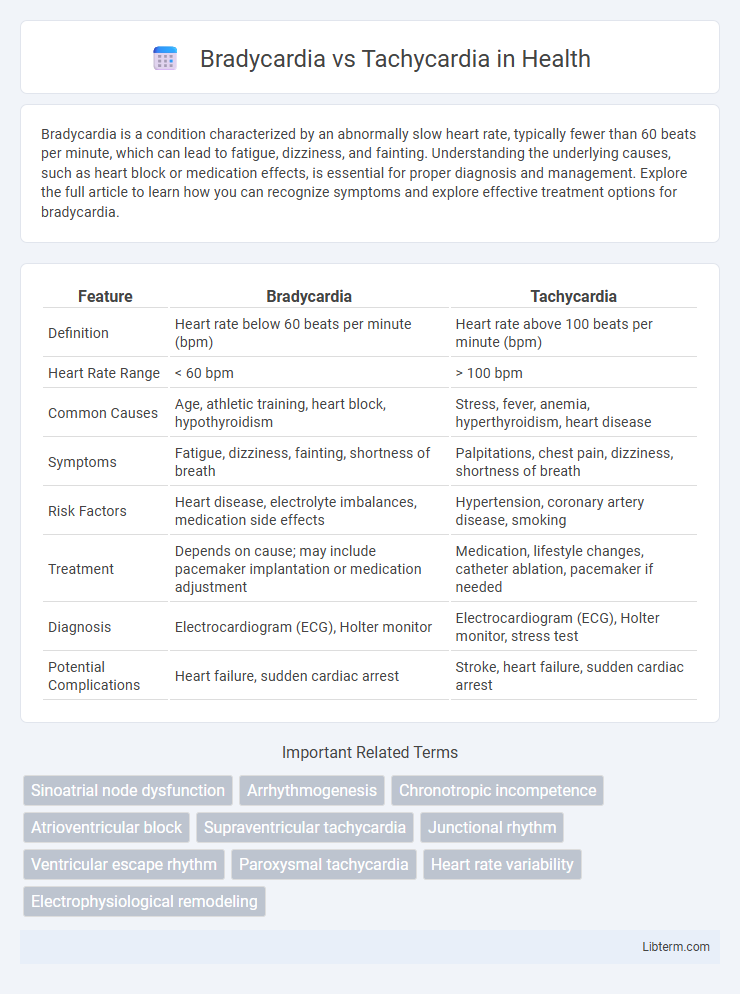
| Feature | Bradycardia | Tachycardia |
|---|---|---|
| Definition | Heart rate below 60 beats per minute (bpm) | Heart rate above 100 beats per minute (bpm) |
| Heart Rate Range | < 60 bpm | > 100 bpm |
| Common Causes | Age, athletic training, heart block, hypothyroidism | Stress, fever, anemia, hyperthyroidism, heart disease |
| Symptoms | Fatigue, dizziness, fainting, shortness of breath | Palpitations, chest pain, dizziness, shortness of breath |
| Risk Factors | Heart disease, electrolyte imbalances, medication side effects | Hypertension, coronary artery disease, smoking |
| Treatment | Depends on cause; may include pacemaker implantation or medication adjustment | Medication, lifestyle changes, catheter ablation, pacemaker if needed |
| Diagnosis | Electrocardiogram (ECG), Holter monitor | Electrocardiogram (ECG), Holter monitor, stress test |
| Potential Complications | Heart failure, sudden cardiac arrest | Stroke, heart failure, sudden cardiac arrest |
Understanding Bradycardia and Tachycardia
Bradycardia is a condition characterized by a resting heart rate below 60 beats per minute, often causing fatigue, dizziness, or fainting due to insufficient blood flow. Tachycardia involves a resting heart rate above 100 beats per minute, which can lead to palpitations, shortness of breath, and increased risk of heart complications. Both conditions disrupt normal cardiac rhythm, requiring medical evaluation to determine underlying causes such as heart disease, electrolyte imbalances, or medication effects.
Causes of Bradycardia
Bradycardia is primarily caused by aging-related degeneration of the heart's electrical system, hypothyroidism, or electrolyte imbalances such as hyperkalemia. Other causes include medications like beta-blockers, heart block due to ischemic heart disease, and conditions such as sleep apnea or inflammatory diseases affecting the myocardium. Identifying the underlying cause is essential for targeted treatment and preventing complications associated with dangerously slow heart rates.
Causes of Tachycardia
Tachycardia occurs due to various causes such as heart-related conditions like hypertension, coronary artery disease, and cardiomyopathy, as well as non-cardiac factors including fever, anemia, hyperthyroidism, and stimulant use like caffeine or nicotine. It can also result from stress, dehydration, or electrolyte imbalances that disrupt normal heart rhythm. Identifying the underlying cause is crucial for effective treatment and management of tachycardia to prevent complications like heart failure or stroke.
Symptoms: Bradycardia vs Tachycardia
Bradycardia symptoms include fatigue, dizziness, shortness of breath, and fainting due to a heart rate below 60 beats per minute. Tachycardia manifests with palpitations, chest pain, rapid heartbeat exceeding 100 beats per minute, and sometimes dizziness or lightheadedness. Both conditions can lead to complications like fainting or heart failure if untreated.
Diagnostic Methods for Heart Rate Disorders
Electrocardiogram (ECG) remains the gold standard for diagnosing bradycardia and tachycardia, providing detailed information about heart rate and rhythm abnormalities. Holter monitoring offers continuous, real-time assessment over 24 to 48 hours, capturing intermittent arrhythmias that might be missed in a standard ECG. Electrophysiological studies (EPS) are utilized for in-depth evaluation and localization of abnormal electrical pathways, particularly in complex or symptomatic cases.
Potential Health Risks and Complications
Bradycardia, defined as a heart rate below 60 beats per minute, can lead to fatigue, dizziness, and in severe cases, heart failure due to inadequate blood flow to organs. Tachycardia, characterized by a heart rate exceeding 100 beats per minute, increases the risk of stroke, heart attack, and sudden cardiac arrest because of sustained high cardiac workload and reduced coronary perfusion. Both conditions may cause arrhythmias and require medical evaluation to prevent critical complications.
Treatment Options for Bradycardia
Treatment for bradycardia primarily involves addressing the underlying cause, which can include medication adjustments or the management of conditions like hypothyroidism or electrolyte imbalances. In cases where bradycardia leads to significant symptoms or hemodynamic instability, implantation of a pacemaker is the most effective long-term solution. Temporary treatments may also include the administration of atropine or temporary transcutaneous pacing to stabilize heart rate until definitive therapy is established.
Treatment Options for Tachycardia
Tachycardia treatment options primarily include medications such as beta-blockers, calcium channel blockers, and antiarrhythmic drugs to control heart rate and rhythm. Invasive procedures like catheter ablation, which targets and destroys abnormal heart tissue causing rapid beats, offer a long-term solution for certain types of tachycardia. Implantable devices like pacemakers or defibrillators may be necessary for patients with recurrent or life-threatening tachyarrhythmias to maintain normal heart rhythm.
Lifestyle Adjustments and Prevention
Lifestyle adjustments for bradycardia often involve monitoring heart rate and avoiding medications that slow the heart, while incorporating regular exercise, a balanced diet, and stress management to support cardiac function. Prevention of tachycardia focuses on maintaining a healthy weight, limiting caffeine and alcohol intake, managing stress effectively, and controlling underlying conditions such as hypertension and thyroid disorders. Both conditions benefit from routine cardiovascular check-ups and adherence to prescribed treatments to reduce complications and improve heart health.
When to Seek Medical Attention
Seek medical attention for bradycardia if symptoms include dizziness, fatigue, chest pain, or fainting, as these may indicate an underlying heart condition requiring prompt evaluation. Tachycardia warrants emergency care when accompanied by shortness of breath, severe chest pain, or loss of consciousness, signaling potential cardiac arrhythmias or heart failure. Persistent or worsening heart rate abnormalities should be assessed by a healthcare professional to prevent complications.
Bradycardia Infographic
 libterm.com
libterm.com