Nonfunctional pancreatic neuroendocrine tumors (PNETs), unlike insulinomas, do not produce excess insulin, leading to delayed diagnosis due to the absence of hypoglycemic symptoms. These tumors often present with nonspecific symptoms or are found incidentally during imaging for other conditions. Explore this article to better understand the distinctions, symptoms, and treatment options for your knowledge on pancreatic neuroendocrine tumors.
Table of Comparison
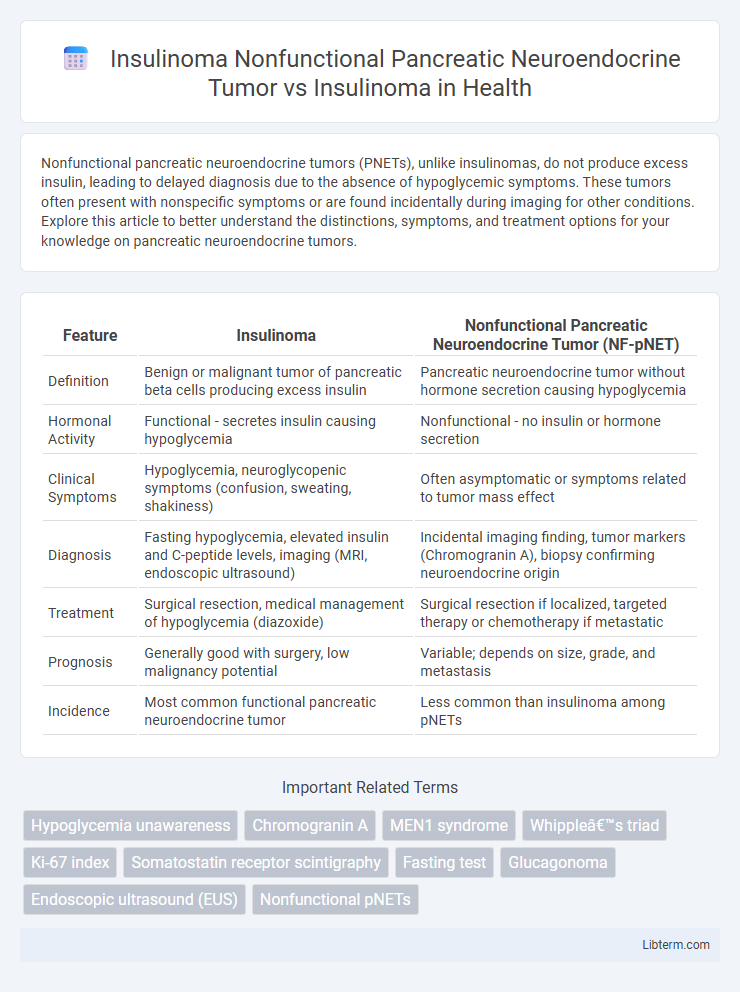
| Feature | Insulinoma | Nonfunctional Pancreatic Neuroendocrine Tumor (NF-pNET) |
|---|---|---|
| Definition | Benign or malignant tumor of pancreatic beta cells producing excess insulin | Pancreatic neuroendocrine tumor without hormone secretion causing hypoglycemia |
| Hormonal Activity | Functional - secretes insulin causing hypoglycemia | Nonfunctional - no insulin or hormone secretion |
| Clinical Symptoms | Hypoglycemia, neuroglycopenic symptoms (confusion, sweating, shakiness) | Often asymptomatic or symptoms related to tumor mass effect |
| Diagnosis | Fasting hypoglycemia, elevated insulin and C-peptide levels, imaging (MRI, endoscopic ultrasound) | Incidental imaging finding, tumor markers (Chromogranin A), biopsy confirming neuroendocrine origin |
| Treatment | Surgical resection, medical management of hypoglycemia (diazoxide) | Surgical resection if localized, targeted therapy or chemotherapy if metastatic |
| Prognosis | Generally good with surgery, low malignancy potential | Variable; depends on size, grade, and metastasis |
| Incidence | Most common functional pancreatic neuroendocrine tumor | Less common than insulinoma among pNETs |
Overview of Pancreatic Neuroendocrine Tumors
Pancreatic neuroendocrine tumors (PNETs) are a heterogeneous group of neoplasms arising from the islet cells of the pancreas, classified as functional or nonfunctional based on hormone secretion. Insulinomas are functional PNETs that secrete insulin, causing hypoglycemia, whereas nonfunctional pancreatic neuroendocrine tumors (NF-PNETs) lack hormone hypersecretion and often present with nonspecific symptoms or mass effects. NF-PNETs generally have a more indolent course but are diagnosed later than insulinomas due to the absence of hormonal syndromes, impacting treatment strategies and prognosis.
Defining Insulinoma: Functional vs Nonfunctional Tumors
Insulinoma is a type of pancreatic neuroendocrine tumor (PNET) characterized by insulin secretion, leading to hypoglycemia and classified as a functional tumor due to its hormone-producing activity. Nonfunctional pancreatic neuroendocrine tumors, including nonfunctional insulinomas, do not secrete significant amounts of insulin or other hormones, often resulting in delayed diagnosis due to lack of hormonal symptoms. Distinguishing between functional insulinomas and nonfunctional PNETs relies on clinical presentation, biochemical testing for insulin levels, and imaging studies to guide appropriate management and prognostic assessment.
Epidemiology of Insulinoma and Nonfunctional PNETs
Insulinomas represent the most common functional pancreatic neuroendocrine tumors (PNETs) with an incidence of approximately 1 to 4 cases per million per year, predominantly affecting adults aged 40 to 60. Nonfunctional PNETs, in contrast, are more prevalent overall and often diagnosed at a later stage due to the absence of hormone-related symptoms, with an incidence estimated at 0.8 to 2 per 100,000 individuals annually. Epidemiologic data indicate nonfunctional tumors comprise roughly 60-90% of all PNETs, making them a significant clinical challenge despite lower rates of hormone secretion compared to insulinomas.
Pathophysiological Differences Between Insulinoma and Nonfunctional Tumors
Insulinomas are functional pancreatic neuroendocrine tumors (PNETs) that secrete insulin, leading to hypoglycemia, whereas nonfunctional pancreatic neuroendocrine tumors (NF-PNETs) do not produce hormones or cause clinical syndromes. Pathophysiologically, insulinomas arise from beta cells with autonomous insulin secretion disrupting glucose homeostasis, while NF-PNETs lack hormone secretion and often present late due to mass effects rather than metabolic symptoms. The difference in hormone activity critically influences tumor behavior, clinical presentation, and management strategies.
Clinical Presentation and Symptomatology
Nonfunctional pancreatic neuroendocrine tumors (NF-PNETs) typically present with vague abdominal pain or are incidentally discovered, as they do not secrete active hormones causing hypoglycemia, unlike insulinomas. Insulinomas manifest primarily through neuroglycopenic symptoms such as confusion, diaphoresis, and tremors due to endogenous hyperinsulinemic hypoglycemia, often following fasting or exercise. Clinical diagnosis of insulinoma hinges on correlating Whipple's triad with elevated insulin, C-peptide, and proinsulin levels during a supervised 72-hour fast, whereas NF-PNETs require imaging for tumor identification without specific hypoglycemic symptomatology.
Diagnostic Approaches and Biomarker Profiles
Insulinoma nonfunctional pancreatic neuroendocrine tumors (NF-PNETs) lack the characteristic hypoglycemia caused by insulin hypersecretion, requiring imaging techniques such as multiphasic CT, MRI, and somatostatin receptor scintigraphy for localization. Biomarker profiles differ as insulinomas exhibit elevated serum insulin and C-peptide levels during hypoglycemic episodes, whereas NF-PNETs show normal insulin but may express markers like chromogranin A and neuron-specific enolase. Advanced diagnostic approaches integrate endoscopic ultrasound-guided fine-needle aspiration and biochemical assays to differentiate functional insulinomas from nonfunctional pancreatic neuroendocrine tumors accurately.
Imaging Techniques for Tumor Localization
Insulinoma Nonfunctional Pancreatic Neuroendocrine Tumors (NF-PNETs) often require advanced imaging techniques such as contrast-enhanced MRI and somatostatin receptor scintigraphy (SRS) to improve tumor localization due to their lack of clinical hypoglycemia symptoms. In contrast, functional insulinomas are typically localized using endoscopic ultrasound (EUS) and 68Ga-DOTATATE PET/CT, which provide higher sensitivity in detecting small pancreatic lesions. Multiphasic CT scans remain a valuable imaging modality for both types, offering detailed vascular mapping essential for surgical planning.
Treatment Modalities: Surgical and Medical Management
Nonfunctional pancreatic neuroendocrine tumors (PNETs), unlike insulinomas which secrete insulin causing hypoglycemia, often present later due to lack of hormonal symptoms and require surgical resection for localized disease to achieve cure. Medical management for nonfunctional PNETs includes somatostatin analogs like octreotide or lanreotide to control tumor growth, along with targeted therapies such as everolimus and sunitinib for advanced or metastatic cases. Insulinomas primarily undergo enucleation or partial pancreatectomy for resection, with diazoxide and octreotide utilized to medically manage hypoglycemic episodes when surgery is contraindicated or delayed.
Prognosis and Long-Term Outcomes
Nonfunctional pancreatic neuroendocrine tumors (PNETs), including nonfunctional insulinomas, generally have a poorer prognosis and higher rates of metastasis compared to functional insulinomas, which tend to be diagnosed earlier due to hypoglycemic symptoms. Functional insulinomas typically exhibit better long-term outcomes with surgical resection, achieving high survival rates exceeding 90% at 5 years. Nonfunctional PNETs often require more extensive management and have lower 5-year survival, ranging from 40% to 60%, due to delayed diagnosis and increased tumor burden.
Surveillance and Follow-Up Strategies
Surveillance and follow-up for Nonfunctional Pancreatic Neuroendocrine Tumors (NF-PNETs) involve regular imaging with MRI or CT scans every 6-12 months to monitor tumor growth and metastasis, as these tumors often present asymptomatically and may progress silently. Insulinomas require more frequent biochemical monitoring of fasting insulin and glucose levels alongside imaging every 3-6 months, given their functional nature causing hypoglycemia and higher risk of symptomatic recurrence. Long-term management for both includes tailored follow-up based on tumor size, grade, and resection status, with aggressive tumors necessitating closer surveillance to detect early progression or recurrence.
Insulinoma Nonfunctional Pancreatic Neuroendocrine Tumor Infographic
 libterm.com
libterm.com