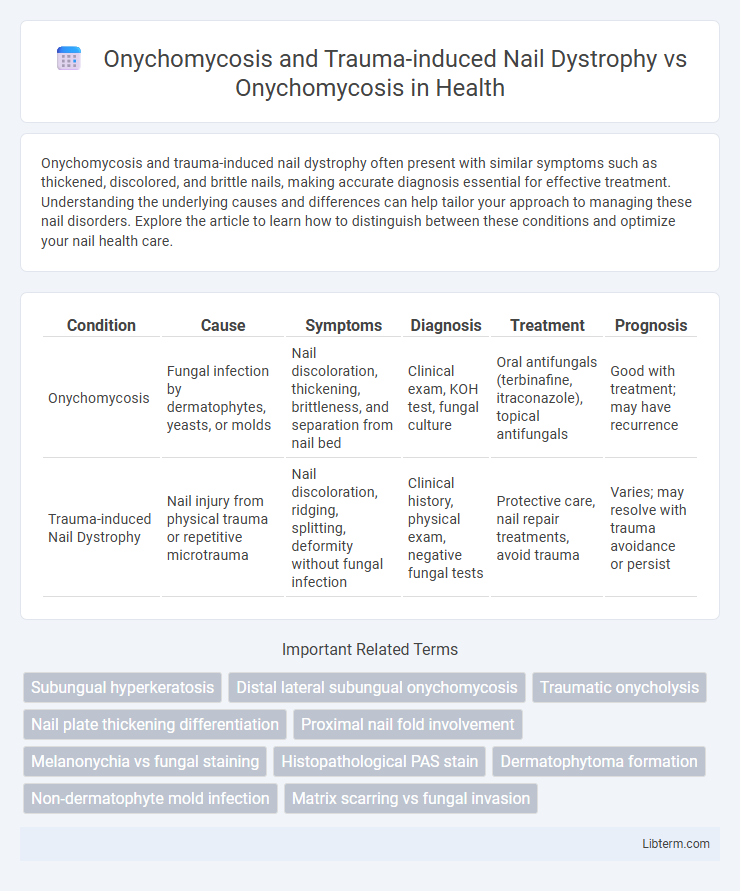
Onychomycosis and trauma-induced nail dystrophy often present with similar symptoms such as thickened, discolored, and brittle nails, making accurate diagnosis essential for effective treatment. Understanding the underlying causes and differences can help tailor your approach to managing these nail disorders. Explore the article to learn how to distinguish between these conditions and optimize your nail health care.
Table of Comparison
| Condition | Cause | Symptoms | Diagnosis | Treatment | Prognosis |
|---|---|---|---|---|---|
| Onychomycosis | Fungal infection by dermatophytes, yeasts, or molds | Nail discoloration, thickening, brittleness, and separation from nail bed | Clinical exam, KOH test, fungal culture | Oral antifungals (terbinafine, itraconazole), topical antifungals | Good with treatment; may have recurrence |
| Trauma-induced Nail Dystrophy | Nail injury from physical trauma or repetitive microtrauma | Nail discoloration, ridging, splitting, deformity without fungal infection | Clinical history, physical exam, negative fungal tests | Protective care, nail repair treatments, avoid trauma | Varies; may resolve with trauma avoidance or persist |
Understanding Onychomycosis: Causes and Risk Factors
Onychomycosis, a fungal infection of the nails, primarily results from dermatophytes, yeasts, and non-dermatophyte molds affecting the nail bed and plate. Risk factors include chronic exposure to moist environments, immunosuppression, diabetes mellitus, peripheral vascular disease, and repeated nail trauma. Trauma-induced nail dystrophy mimics onychomycosis symptoms but is caused by physical injury disrupting nail integrity, leading to secondary infections and diagnostic challenges.
Clinical Presentation of Onychomycosis
Onychomycosis commonly presents with thickened, discolored, and brittle nails, often showing subungual hyperkeratosis and distal onycholysis. Trauma-induced nail dystrophy may mimic onychomycosis but typically exhibits irregular nail plate deformities localized to the area of injury without fungal invasion. Distinguishing the clinical presentation of onychomycosis from trauma-induced changes relies on the presence of fungal elements confirmed by microscopy or culture.
What is Trauma-induced Nail Dystrophy?
Trauma-induced Nail Dystrophy refers to nail abnormalities caused by physical injury, resulting in nail discoloration, thickening, and deformation that can mimic onychomycosis symptoms. Unlike fungal infections, this condition arises from repetitive or acute trauma that disrupts nail growth and structure without microbial involvement. Accurate differentiation between trauma-induced changes and onychomycosis is essential for effective treatment, often requiring clinical evaluation and diagnostic tests such as fungal cultures or microscopy.
Differentiating Onychomycosis from Trauma-induced Nail Dystrophy
Differentiating onychomycosis from trauma-induced nail dystrophy relies on clinical examination and diagnostic tests such as KOH microscopy, fungal culture, and nail biopsy. Onychomycosis typically presents with yellowish discoloration, subungual hyperkeratosis, and nail plate thickening, whereas trauma-induced dystrophy often shows irregular nail plate ridging, splitting, and hemorrhages without fungal elements. Accurate identification is crucial for targeted antifungal therapy versus conservative management or trauma protection strategies.
Key Diagnostic Criteria for Onychomycosis
Onychomycosis diagnosis relies on clinical features such as nail discoloration, thickening, and subungual debris, confirmed by positive direct microscopy and culture of nail clippings to identify fungal organisms. Trauma-induced nail dystrophy often mimics onychomycosis but lacks fungal elements on mycological tests and may present with irregular nail plate changes and hemorrhages stemming from mechanical injury. Key diagnostic criteria for onychomycosis emphasize laboratory confirmation to differentiate it from trauma-induced nail dystrophy and avoid misdiagnosis.
Common Features of Trauma-related Nail Changes
Onychomycosis and trauma-induced nail dystrophy share several common clinical features including nail discoloration, thickening, and distal onycholysis. Both conditions often present with subungual debris and irregular nail surface texture, complicating differential diagnosis without mycological testing. Nail plate brittleness and splitting are frequently observed in trauma-related nail changes, similar to the keratin degradation seen in fungal infections.
Diagnostic Tools: Lab Tests and Imaging
Diagnosing onychomycosis involves laboratory tests such as potassium hydroxide (KOH) preparation, fungal culture, and polymerase chain reaction (PCR) to detect fungal elements, while trauma-induced nail dystrophy lacks fungal presence and may require clinical correlation. Imaging techniques like dermoscopy and high-frequency ultrasound can aid in distinguishing onychomycosis from trauma by revealing subungual hyperkeratosis or nail plate irregularities specific to fungal infection. Mycological examination remains the gold standard to confirm fungal etiology, whereas trauma diagnosis relies more on patient history and the absence of fungal markers in lab tests.
Overlapping Symptoms: Similarities and Differences
Onychomycosis and trauma-induced nail dystrophy both present with nail thickening, discoloration, and brittleness, making clinical differentiation challenging. Onychomycosis typically exhibits subungual debris and slow nail plate separation, while trauma-induced dystrophy often shows localized nail irregularities and proximal nail bed hemorrhages. Diagnostic tools like fungal culture and dermoscopy aid in distinguishing fungal infection from mechanical injury by identifying fungal elements or specific trauma patterns.
Treatment Approaches: Fungal vs. Traumatic Nail Conditions
Treatment approaches for onychomycosis primarily involve systemic antifungal agents such as terbinafine or itraconazole paired with topical treatments like ciclopirox or efinaconazole to eradicate fungal pathogens and restore nail integrity. In contrast, trauma-induced nail dystrophy requires management focused on protecting the nail from further injury, addressing underlying causes like repetitive mechanical stress, and possibly employing topical corticosteroids or nail repair techniques to promote healing. Accurate diagnosis through mycological testing is essential to differentiate fungal infections from traumatic nail conditions and guide appropriate therapeutic strategies.
Prevention and Long-term Management Strategies
Prevention and long-term management of Onychomycosis require maintaining proper nail hygiene, avoiding prolonged moisture exposure, and using antifungal treatments consistently to prevent recurrence. Trauma-induced Nail Dystrophy management focuses on protecting nails from repeated injury, proper wound care, and monitoring for secondary infections, which can mimic or exacerbate Onychomycosis symptoms. Both conditions benefit from regular dermatological consultations to tailor treatments, address underlying causes, and implement lifestyle modifications that promote nail health.
Onychomycosis and Trauma-induced Nail Dystrophy Infographic
 libterm.com
libterm.com