Pneumothorax occurs when air leaks into the space between the lung and chest wall, causing the lung to collapse partially or fully. Symptoms often include sudden chest pain and shortness of breath, requiring prompt medical attention to prevent complications. Discover essential information on causes, symptoms, and treatment options to protect your respiratory health by reading the full article.
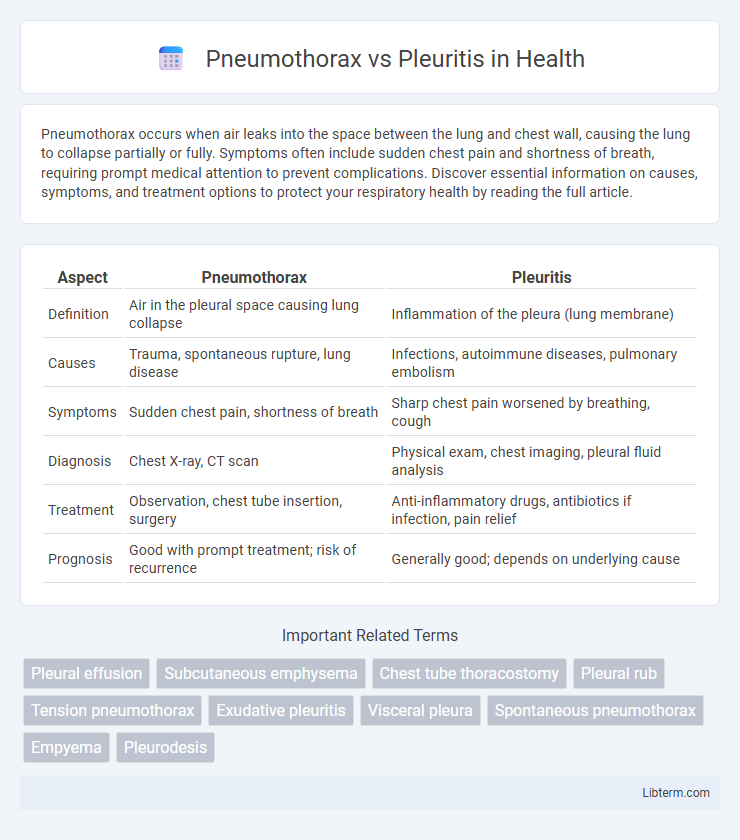
Table of Comparison
| Aspect | Pneumothorax | Pleuritis |
|---|---|---|
| Definition | Air in the pleural space causing lung collapse | Inflammation of the pleura (lung membrane) |
| Causes | Trauma, spontaneous rupture, lung disease | Infections, autoimmune diseases, pulmonary embolism |
| Symptoms | Sudden chest pain, shortness of breath | Sharp chest pain worsened by breathing, cough |
| Diagnosis | Chest X-ray, CT scan | Physical exam, chest imaging, pleural fluid analysis |
| Treatment | Observation, chest tube insertion, surgery | Anti-inflammatory drugs, antibiotics if infection, pain relief |
| Prognosis | Good with prompt treatment; risk of recurrence | Generally good; depends on underlying cause |
Introduction to Pneumothorax and Pleuritis
Pneumothorax is a medical condition characterized by the presence of air in the pleural space, leading to lung collapse and acute respiratory distress. Pleuritis, also known as pleurisy, involves inflammation of the pleura, the membrane surrounding the lungs, causing sharp chest pain and difficulty breathing. Both conditions affect the pleural cavity but differ fundamentally in etiology, symptoms, and management.
Definition and Overview
Pneumothorax is the presence of air in the pleural space causing lung collapse, often resulting from trauma or spontaneous rupture of lung tissue. Pleuritis, also known as pleurisy, is inflammation of the pleura, the membrane surrounding the lungs, frequently caused by infections, autoimmune diseases, or lung conditions. Both conditions affect the pleural cavity, but pneumothorax primarily involves air leakage, while pleuritis involves inflammatory pain and pleural thickening.
Etiology: Causes and Risk Factors
Pneumothorax primarily results from trauma, spontaneous alveolar rupture, or underlying lung diseases such as COPD, cystic fibrosis, and asthma, with risk factors including smoking, tall thin body habitus, and mechanical ventilation. Pleuritis, or pleurisy, is typically caused by viral infections, bacterial pneumonia, tuberculosis, autoimmune diseases like lupus, and pulmonary embolism, with risk factors involving recent respiratory infections, autoimmune disorders, and chest trauma. Understanding the distinct etiologies aids in accurate diagnosis and targeted treatment strategies.
Pathophysiology: How the Conditions Develop
Pneumothorax develops when air accumulates in the pleural space due to a breach in the lung surface or chest wall, causing lung collapse and impaired gas exchange. Pleuritis, or pleurisy, arises from inflammation of the pleural layers, often triggered by infections, autoimmune disorders, or pulmonary embolism, leading to pleural thickening and pain from friction during respiration. Both conditions disrupt normal pleural function but differ fundamentally in their underlying mechanisms--air accumulation versus inflammatory response.
Clinical Presentation: Signs and Symptoms
Pneumothorax typically presents with sudden onset of sharp, unilateral chest pain and dyspnea, accompanied by reduced breath sounds and hyperresonance on the affected side during physical examination. Pleuritis manifests as pleuritic chest pain that worsens with deep breathing or coughing, often accompanied by a pleural friction rub auscultated over the inflamed area. Both conditions may present with tachypnea and signs of respiratory distress, but pneumothorax frequently shows tracheal deviation and decreased chest wall movement in severe cases.
Diagnostic Approaches and Imaging
Diagnostic approaches for pneumothorax primarily involve chest X-rays and computed tomography (CT) scans, which effectively detect air presence in the pleural cavity and lung collapse. Pleuritis diagnosis relies on clinical evaluation complemented by chest X-rays, ultrasound, and sometimes CT imaging to identify pleural thickening, fluid accumulation, or inflammation. Ultrasound is increasingly valuable in assessing pleural effusions and guiding thoracentesis, aiding differentiation between pneumothorax and pleuritis in complex cases.
Treatment Options and Management Strategies
Treatment options for pneumothorax primarily involve needle aspiration, chest tube insertion, and in severe cases, surgical intervention such as video-assisted thoracoscopic surgery (VATS) to re-expand the lung and prevent recurrence. Pleuritis management focuses on addressing the underlying cause, often requiring anti-inflammatory medications, analgesics, and treating infections with antibiotics if bacterial pleurisy is diagnosed. Both conditions may require supportive care including oxygen therapy and monitoring to prevent complications like respiratory distress or chronic pleural thickening.
Complications and Prognosis
Pneumothorax complications often include respiratory distress, tension pneumothorax, and potential cardiac arrest if untreated, with prognosis varying based on size and underlying lung disease. Pleuritis complications may involve pleural effusion, fibrosis, and chronic pain, impacting respiratory function and quality of life. Prognosis in pneumothorax generally improves with prompt intervention, while pleuritis outcome depends on the cause and effectiveness of anti-inflammatory treatment.
Key Differences Between Pneumothorax and Pleuritis
Pneumothorax involves the presence of air in the pleural cavity causing lung collapse, whereas pleuritis is inflammation of the pleura leading to sharp chest pain and pleural friction. Pneumothorax typically presents with sudden onset dyspnea and decreased breath sounds, while pleuritis manifests with localized pleuritic pain that worsens with respiration. Diagnostic imaging for pneumothorax reveals air pockets on chest X-ray or CT scan, contrasting with pleuritis where imaging may show pleural thickening or effusion without lung collapse.
Prevention and Patient Education
Preventing pneumothorax involves avoiding risk factors such as smoking, managing underlying lung conditions, and exercising caution during activities that increase chest trauma risk. Patient education for pleuritis emphasizes recognizing early symptoms like sharp chest pain during breathing, adhering to prescribed treatments, and understanding the importance of treating underlying infections or autoimmune disorders. Both conditions benefit from prompt medical attention and lifestyle adjustments to reduce recurrence and complications.
Pneumothorax Infographic
 libterm.com
libterm.com