Pneumonia is a lung infection causing inflammation and fluid buildup in the air sacs, leading to symptoms like cough, fever, and difficulty breathing. It can affect people of all ages, with higher risks for infants, the elderly, and those with weakened immune systems. Discover how to recognize, prevent, and treat pneumonia effectively by reading the rest of the article.
Table of Comparison
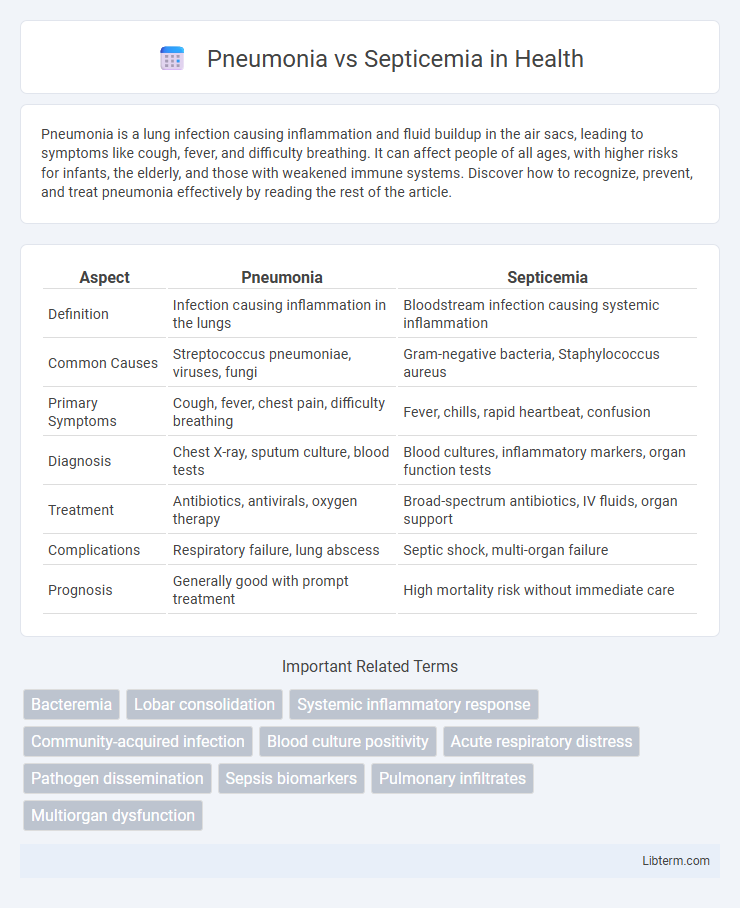
| Aspect | Pneumonia | Septicemia |
|---|---|---|
| Definition | Infection causing inflammation in the lungs | Bloodstream infection causing systemic inflammation |
| Common Causes | Streptococcus pneumoniae, viruses, fungi | Gram-negative bacteria, Staphylococcus aureus |
| Primary Symptoms | Cough, fever, chest pain, difficulty breathing | Fever, chills, rapid heartbeat, confusion |
| Diagnosis | Chest X-ray, sputum culture, blood tests | Blood cultures, inflammatory markers, organ function tests |
| Treatment | Antibiotics, antivirals, oxygen therapy | Broad-spectrum antibiotics, IV fluids, organ support |
| Complications | Respiratory failure, lung abscess | Septic shock, multi-organ failure |
| Prognosis | Generally good with prompt treatment | High mortality risk without immediate care |
Introduction to Pneumonia and Septicemia
Pneumonia is an inflammatory condition of the lung primarily caused by bacterial, viral, or fungal infections, leading to symptoms such as cough, fever, and difficulty breathing. Septicemia, also known as blood poisoning, occurs when pathogens enter the bloodstream, triggering a systemic inflammatory response that can result in sepsis, organ dysfunction, and potentially fatal outcomes. Both conditions require prompt diagnosis and treatment to prevent severe complications and improve patient survival rates.
Understanding Pneumonia: Causes and Risk Factors
Pneumonia is an infection that inflames the air sacs in one or both lungs, commonly caused by bacteria such as Streptococcus pneumoniae, viruses, or fungi. Risk factors include advanced age, chronic respiratory diseases, weakened immune systems, smoking, and recent respiratory infections. Understanding these causes and risk factors is essential for early diagnosis and effective treatment to prevent complications like septicemia, a severe bloodstream infection.
Septicemia Explained: Origins and Triggers
Septicemia, also known as blood poisoning, originates from a bacterial infection entering the bloodstream, often triggered by infections such as pneumonia, urinary tract infections, or wounds. The presence of bacteria in the blood leads to systemic inflammatory response syndrome (SIRS), causing widespread inflammation, tissue damage, and potentially septic shock. Early recognition of septicemia's triggers, including pneumonia-causing pathogens like Streptococcus pneumoniae, is crucial for prompt antibiotic treatment and prevention of fatal complications.
Key Differences Between Pneumonia and Septicemia
Pneumonia primarily affects the lungs, causing inflammation and fluid buildup in the alveoli, leading to symptoms such as cough, fever, and difficulty breathing. Septicemia, also known as sepsis, is a systemic bloodstream infection resulting from bacteria entering the blood, triggering widespread inflammation and potentially causing organ failure. While pneumonia is a localized respiratory infection, septicemia represents a critical progression where infection spreads systemically, necessitating immediate intervention to prevent septic shock and multi-organ dysfunction.
Signs and Symptoms: Pneumonia vs Septicemia
Pneumonia typically presents with signs such as productive cough, chest pain, shortness of breath, high fever, and crackling sounds in the lungs. Septicemia, or bloodstream infection, manifests through symptoms like high fever, chills, rapid heartbeat, confusion, and low blood pressure, indicating systemic infection. Both conditions can cause fever and fatigue, but pneumonia's respiratory symptoms contrast with septicemia's signs of widespread inflammation and organ dysfunction.
Diagnostic Approaches for Pneumonia and Septicemia
Diagnostic approaches for pneumonia commonly include chest X-rays, sputum cultures, and blood tests to identify causative pathogens and assess lung involvement. Septicemia diagnosis relies heavily on blood cultures to detect the presence of bacteria or fungi in the bloodstream, alongside biomarkers like procalcitonin and C-reactive protein levels. Both conditions benefit from imaging studies and laboratory tests, but pneumonia diagnosis emphasizes respiratory samples, whereas septicemia diagnosis focuses on systemic infection markers and blood pathogen identification.
Treatment Strategies: Comparing Both Conditions
Treatment strategies for pneumonia primarily involve targeted antibiotic therapy based on the causative pathogen, supportive care such as oxygen supplementation, and in severe cases, mechanical ventilation. Septicemia requires aggressive intravenous broad-spectrum antibiotics, fluid resuscitation to maintain hemodynamic stability, and close monitoring in an intensive care setting to prevent organ failure. Both conditions demand early diagnosis and prompt treatment to reduce mortality, but septicemia often necessitates more complex interventions including vasopressors and potential source control through surgery.
Potential Complications and Prognosis
Pneumonia can lead to complications such as pleural effusion, lung abscess, acute respiratory distress syndrome (ARDS), and sepsis, with prognosis largely dependent on the patient's age, comorbidities, and timeliness of antibiotic treatment. Septicemia, often arising from untreated infections like pneumonia, can progress to septic shock, multi-organ failure, and death, with early diagnosis and aggressive management being critical to improving survival rates. Both conditions require prompt medical intervention to reduce the risk of severe complications and improve long-term outcomes.
Prevention Tips for Pneumonia and Septicemia
Effective prevention of pneumonia includes regular vaccination against pneumococcal bacteria and influenza, practicing good hand hygiene, avoiding smoking, and maintaining a healthy immune system through proper nutrition and exercise. Preventing septicemia involves early treatment of infections, proper wound care, timely use of antibiotics for bacterial infections, and infection control measures in healthcare settings to reduce bloodstream infections. Both conditions benefit from prompt medical attention and managing chronic illnesses to reduce the risk of severe complications.
Frequently Asked Questions about Pneumonia and Septicemia
Pneumonia is a lung infection characterized by symptoms such as cough, fever, chest pain, and difficulty breathing, while septicemia, also known as blood poisoning, results from bacteria entering the bloodstream, leading to systemic inflammation and potential organ failure. Frequently asked questions about pneumonia include its contagiousness, common causes like Streptococcus pneumoniae, and treatment options involving antibiotics and supportive care. For septicemia, common inquiries focus on early signs such as rapid heart rate and fever, risk factors including weakened immune systems, and urgent treatments like intravenous antibiotics and hospitalization.
Pneumonia Infographic
 libterm.com
libterm.com