Anesthesia plays a crucial role in modern medicine by enabling pain-free surgical procedures and ensuring patient comfort and safety. It involves the use of specialized drugs and techniques to temporarily block sensation or consciousness, tailored to the type of surgery and individual patient needs. Explore the rest of the article to learn how anesthesia works and what you can expect during your procedure.
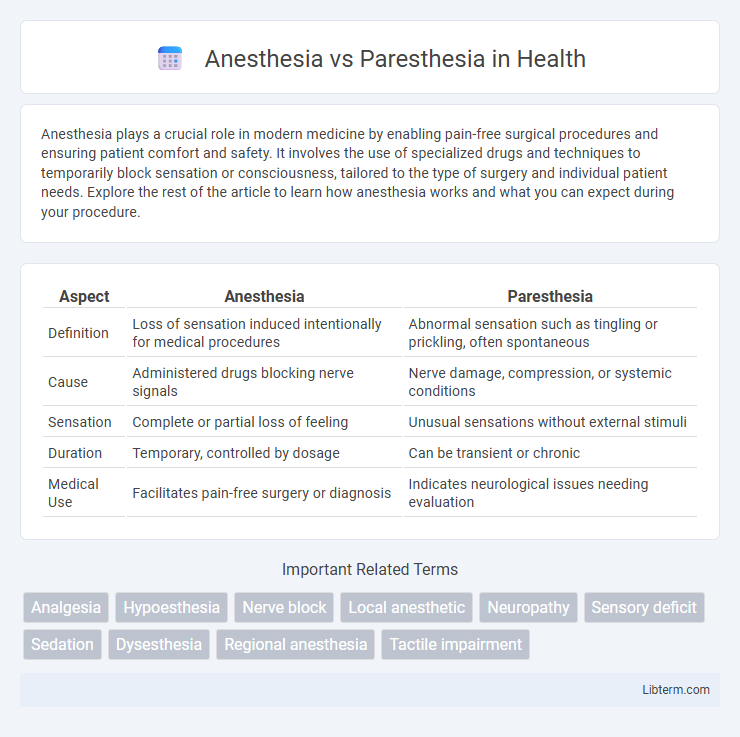
Table of Comparison
| Aspect | Anesthesia | Paresthesia |
|---|---|---|
| Definition | Loss of sensation induced intentionally for medical procedures | Abnormal sensation such as tingling or prickling, often spontaneous |
| Cause | Administered drugs blocking nerve signals | Nerve damage, compression, or systemic conditions |
| Sensation | Complete or partial loss of feeling | Unusual sensations without external stimuli |
| Duration | Temporary, controlled by dosage | Can be transient or chronic |
| Medical Use | Facilitates pain-free surgery or diagnosis | Indicates neurological issues needing evaluation |
Understanding Anesthesia: Definition and Purpose
Anesthesia is a medical technique used to induce a temporary loss of sensation or awareness, allowing patients to undergo surgical procedures without pain or distress. It can be classified into general, regional, and local anesthesia, each targeting different levels of sensory blockade to suit specific medical needs. The primary purpose of anesthesia is to ensure patient comfort, prevent pain, and facilitate safe and effective surgical interventions.
What Is Paresthesia? Key Characteristics
Paresthesia refers to abnormal sensations such as tingling, numbness, or burning often caused by nerve damage or irritation. It is a sensory symptom rather than a condition, frequently experienced in the hands, feet, or face, and can result from conditions like neuropathy, multiple sclerosis, or prolonged pressure on nerves. Unlike anesthesia, which involves a loss of sensation, paresthesia involves altered sensory perception without complete numbness.
Types of Anesthesia: Local, Regional, and General
Local anesthesia targets a specific area to block pain during minor procedures, while regional anesthesia numbs larger body regions by injecting near nerve clusters, commonly used in epidurals or nerve blocks. General anesthesia induces a reversible coma-like state, rendering patients unconscious and insensible to pain for major surgeries. Each anesthesia type varies in depth and scope of pain control, tailored to procedural needs and patient safety.
Common Causes of Paresthesia
Paresthesia commonly results from nerve compression, peripheral neuropathy, or systemic conditions like diabetes mellitus and multiple sclerosis. Physical trauma, repetitive motions, and vitamin deficiencies, particularly B12 deficiency, are also prevalent causes. Identifying the underlying cause is crucial for distinguishing paresthesia from anesthesia, which denotes a complete loss of sensation rather than abnormal sensations.
Mechanisms: How Anesthesia Works
Anesthesia works by blocking nerve signals in the central and peripheral nervous systems, preventing the brain from perceiving pain and other sensations. Local anesthetics inhibit sodium channels on nerve membranes, stopping the initiation and conduction of nerve impulses. In contrast, paresthesia results from nerve irritation or damage, causing abnormal sensations rather than nerve signal blockage.
Pathophysiology of Paresthesia
Paresthesia results from abnormal nerve function causing spontaneous or provoked sensations such as tingling, burning, or numbness, often due to peripheral nerve injury or compression. Pathophysiologically, it involves ectopic nerve discharges, ion channel dysfunction, and altered neuronal excitability, leading to hyperexcitability or abnormal sensory signaling. Unlike anesthesia, which is the loss of sensation caused by nerve signal blockade, paresthesia reflects a dysfunctional sensory pathway producing abnormal sensations without complete sensory loss.
Key Differences Between Anesthesia and Paresthesia
Anesthesia involves the controlled loss of sensation induced by medical agents to prevent pain during surgical procedures, whereas paresthesia refers to abnormal sensations such as tingling or numbness without an external stimulus. Anesthesia is a reversible condition achieved through drugs like local anesthetics or general anesthetics, while paresthesia often results from nerve damage, compression, or neurological disorders. The key difference lies in anesthesia's intentional and temporary sensory suppression compared to paresthesia's involuntary and often pathological nerve-related symptoms.
Clinical Applications: When to Use Anesthesia
Anesthesia is primarily used in clinical settings to induce complete loss of sensation, enabling pain-free surgical procedures such as major operations, dental surgeries, and diagnostic interventions. It is essential when patient immobility, unconsciousness, or deep sedation is required to ensure safety and comfort during invasive treatments. In contrast, paresthesia refers to abnormal sensations like tingling or numbness that are typically symptoms rather than clinical interventions.
Symptoms and Patient Experiences of Paresthesia
Paresthesia involves abnormal sensations such as tingling, numbness, burning, or prickling, often described as "pins and needles," which can cause discomfort or pain for patients. Unlike anesthesia, which is the complete loss of sensation, paresthesia symptoms may persist or fluctuate, potentially affecting daily activities and causing distress. Patient experiences commonly report localized sensory disturbances without paralysis, frequently resulting from nerve irritation or damage.
Prevention and Management Strategies for Both Conditions
Effective prevention of anesthesia and paresthesia involves careful patient assessment, precise injection techniques, and thorough knowledge of anatomical variations to minimize nerve trauma during dental or surgical procedures. Management strategies emphasize early diagnosis and intervention, including pharmacological treatments such as corticosteroids or analgesics, as well as physical therapy to promote nerve regeneration and functional recovery. Continuous patient monitoring and tailored follow-up care are essential to address persistent sensory disturbances and improve clinical outcomes.
Anesthesia Infographic
 libterm.com
libterm.com