Hyponatremia is a condition characterized by low sodium levels in the blood, leading to symptoms such as headache, nausea, and confusion. It often results from excessive fluid intake, certain medications, or underlying medical issues affecting kidney or hormone function. Explore the rest of the article to understand causes, symptoms, and effective treatments for managing your hyponatremia.
Table of Comparison
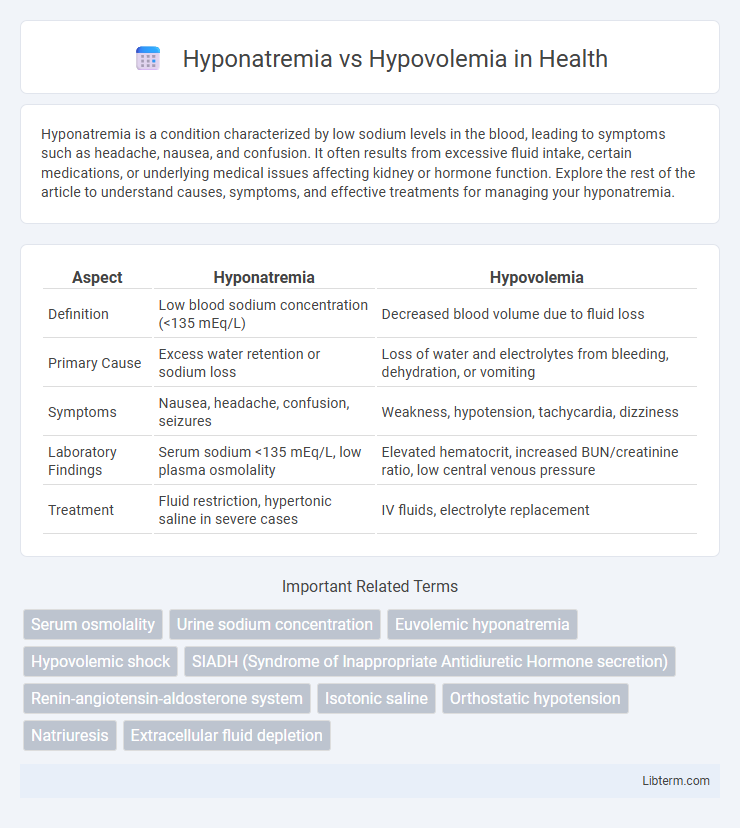
| Aspect | Hyponatremia | Hypovolemia |
|---|---|---|
| Definition | Low blood sodium concentration (<135 mEq/L) | Decreased blood volume due to fluid loss |
| Primary Cause | Excess water retention or sodium loss | Loss of water and electrolytes from bleeding, dehydration, or vomiting |
| Symptoms | Nausea, headache, confusion, seizures | Weakness, hypotension, tachycardia, dizziness |
| Laboratory Findings | Serum sodium <135 mEq/L, low plasma osmolality | Elevated hematocrit, increased BUN/creatinine ratio, low central venous pressure |
| Treatment | Fluid restriction, hypertonic saline in severe cases | IV fluids, electrolyte replacement |
Introduction to Hyponatremia and Hypovolemia
Hyponatremia is characterized by a serum sodium concentration below 135 mEq/L, leading to cellular edema and neurological symptoms due to water imbalance. Hypovolemia refers to a decreased circulating blood volume, resulting in decreased tissue perfusion and potential shock if untreated. Differentiating these conditions is critical, as hyponatremia primarily affects electrolyte balance, while hypovolemia impacts hemodynamic stability.
Definitions and Key Differences
Hyponatremia is a medical condition characterized by low sodium concentration in the blood, typically below 135 mEq/L, while hypovolemia refers to a decreased volume of circulating blood plasma. The key difference lies in their primary pathology: hyponatremia involves electrolyte imbalance affecting cellular function, whereas hypovolemia centers on fluid loss leading to reduced blood volume. Diagnosing hyponatremia requires serum sodium measurement, whereas hypovolemia evaluation focuses on clinical signs of volume depletion and hemodynamic stability.
Causes of Hyponatremia
Hyponatremia occurs due to an imbalance between water and sodium levels in the body, commonly caused by conditions such as Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH), heart failure, liver cirrhosis, and chronic kidney disease. Excessive fluid intake, diuretic use, adrenal insufficiency, and hypothyroidism also contribute to reduced serum sodium concentrations. It is essential to distinguish these causes from hypovolemia, where sodium loss is typically due to renal or extrarenal fluid depletion from vomiting, diarrhea, or hemorrhage.
Causes of Hypovolemia
Hypovolemia is primarily caused by excessive fluid loss due to conditions such as severe vomiting, diarrhea, hemorrhage, or excessive sweating, leading to decreased blood volume. Other common causes include third-space fluid shifts in cases of burn injuries or pancreatitis, and inadequate fluid intake during dehydration or heat exposure. Understanding these causes is crucial for differentiating hypovolemia from hyponatremia, the latter being characterized by low sodium concentration often due to dilutional effects rather than volume loss.
Clinical Presentation and Symptoms
Hyponatremia commonly presents with neurological symptoms such as headache, nausea, confusion, seizures, and in severe cases, coma, due to cerebral edema caused by low serum sodium levels below 135 mEq/L. Hypovolemia manifests primarily with signs of volume depletion including tachycardia, hypotension, dry mucous membranes, decreased skin turgor, and orthostatic hypotension, reflecting reduced circulating blood volume. Differentiating these conditions clinically is crucial since hyponatremia may occur with euvolemia or hypervolemia, but hypovolemia specifically indicates a deficit in extracellular fluid volume affecting hemodynamic stability.
Diagnostic Criteria and Laboratory Findings
Hyponatremia is characterized by a serum sodium concentration below 135 mEq/L, often confirmed through plasma osmolality testing revealing hypoosmolality in true cases, whereas hypovolemia is identified by clinical signs of volume depletion such as decreased skin turgor and orthostatic hypotension. Laboratory findings in hypovolemia typically show elevated blood urea nitrogen to creatinine ratio (>20:1) and increased urine sodium concentration depending on renal salt handling, contrasting with hyponatremia where urine sodium varies and serum osmolality guides diagnosis. Distinguishing these conditions relies on evaluating volume status alongside serum sodium and osmolality, with hypovolemia frequently accompanied by high urine sodium in renal losses or low in extrarenal losses, while hyponatremia involves dilutional or loss-related sodium disturbances.
Pathophysiological Mechanisms
Hyponatremia involves decreased serum sodium concentration due to water retention or sodium loss, disrupting osmotic balance and leading to cellular swelling, especially in the brain. Hypovolemia results from a deficit in extracellular fluid volume, causing decreased blood volume and triggering compensatory mechanisms such as activation of the renin-angiotensin-aldosterone system and sympathetic nervous system. While hyponatremia primarily affects sodium-water homeostasis at the cellular level, hypovolemia primarily impacts vascular volume and perfusion pressure.
Treatment Approaches and Management
Hyponatremia treatment involves careful correction of sodium levels using hypertonic saline in severe cases or fluid restriction for dilutional hyponatremia, while monitoring serum sodium to prevent osmotic demyelination syndrome. Hypovolemia management centers on rapid volume resuscitation with isotonic fluids such as normal saline or lactated Ringer's solution to restore circulatory volume and improve tissue perfusion. Both conditions require tailored intervention based on underlying causes, electrolyte balance, and close hemodynamic monitoring.
Risks and Complications
Hyponatremia, characterized by low sodium levels in the blood, poses risks such as cerebral edema, seizures, and potential neurological damage, especially in severe or rapid onset cases. Hypovolemia, involving decreased blood volume due to fluid loss, increases the risk of hypovolemic shock, acute kidney injury, and multi-organ failure if untreated. Both conditions require prompt diagnosis and management to prevent life-threatening complications related to electrolyte imbalance and inadequate tissue perfusion.
Prevention Strategies and Patient Education
Preventing hyponatremia involves monitoring and regulating fluid intake, especially for patients on diuretics or those with conditions like heart failure or kidney disease, to maintain balanced sodium levels. Hypovolemia prevention centers on adequate hydration and prompt management of conditions causing fluid loss such as vomiting, diarrhea, or excessive sweating. Educating patients about recognizing early symptoms like dizziness, headache, or confusion and maintaining electrolyte balance is crucial for reducing hospitalizations related to these conditions.
Hyponatremia Infographic
 libterm.com
libterm.com