Macrophagic activity plays a crucial role in the immune system by engulfing and digesting cellular debris, pathogens, and foreign substances to protect the body from infections. These specialized cells are essential for maintaining tissue homeostasis and triggering immune responses that support healing. Discover how understanding macrophagic functions can enhance your knowledge of immunity and disease prevention in the rest of this article.
Table of Comparison
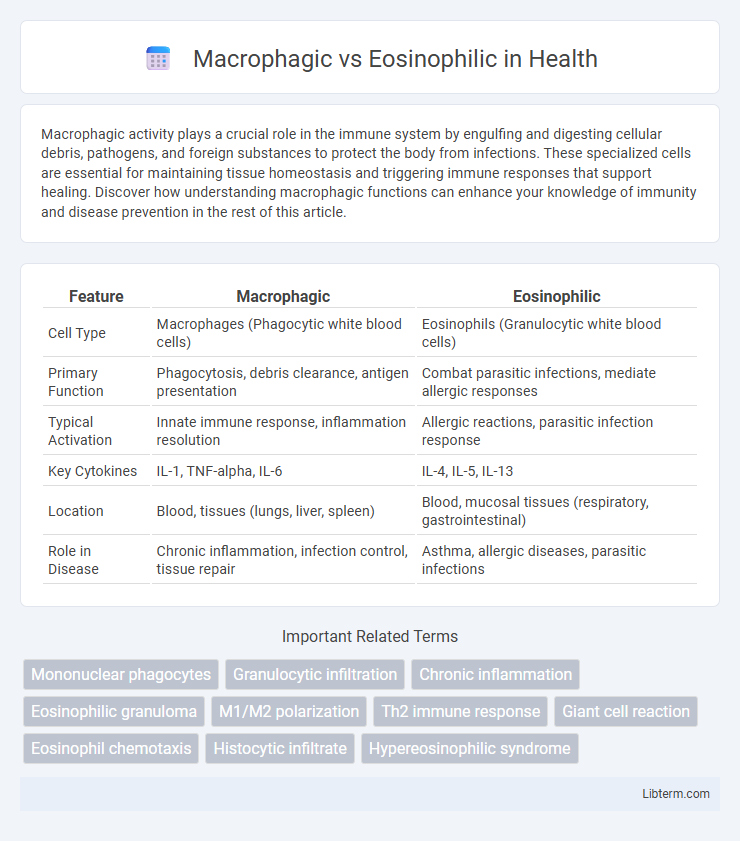
| Feature | Macrophagic | Eosinophilic |
|---|---|---|
| Cell Type | Macrophages (Phagocytic white blood cells) | Eosinophils (Granulocytic white blood cells) |
| Primary Function | Phagocytosis, debris clearance, antigen presentation | Combat parasitic infections, mediate allergic responses |
| Typical Activation | Innate immune response, inflammation resolution | Allergic reactions, parasitic infection response |
| Key Cytokines | IL-1, TNF-alpha, IL-6 | IL-4, IL-5, IL-13 |
| Location | Blood, tissues (lungs, liver, spleen) | Blood, mucosal tissues (respiratory, gastrointestinal) |
| Role in Disease | Chronic inflammation, infection control, tissue repair | Asthma, allergic diseases, parasitic infections |
Introduction to Macrophagic and Eosinophilic Responses
Macrophagic responses involve the activation of macrophages, key immune cells that engulf pathogens and cellular debris to initiate tissue repair and inflammation regulation. Eosinophilic responses are characterized by the recruitment of eosinophils, white blood cells that specialize in combating parasitic infections and modulating allergic reactions through the release of cytotoxic granules. Both responses play distinct roles in immune defense, with macrophages primarily managing innate immunity and eosinophils contributing to adaptive immune pathways.
Defining Macrophagic Activity in the Immune System
Macrophagic activity in the immune system involves the engulfing and digestion of pathogens and cellular debris by macrophages, playing a critical role in innate immunity and tissue homeostasis. This process is characterized by the secretion of pro-inflammatory cytokines, antigen presentation to T cells, and the activation of adaptive immune responses. Unlike eosinophilic responses, which primarily target parasitic infections and mediate allergic inflammation, macrophagic activity centers on phagocytosis and orchestrating a broad immune defense.
Understanding Eosinophilic Function and Mechanisms
Eosinophils are a type of white blood cell primarily involved in combating parasitic infections and mediating allergic responses, characterized by their granules containing cytotoxic proteins such as major basic protein and eosinophil peroxidase. These cells release inflammatory mediators and cytokines that regulate immune responses, tissue remodeling, and contribute to pathogen clearance. Understanding eosinophilic mechanisms highlights their role in chronic inflammation and immune regulation, distinguishing them from macrophages which specialize in phagocytosis and antigen presentation.
Cellular Origins: Macrophages vs Eosinophils
Macrophages originate from monocytes, which are produced in the bone marrow and differentiate into tissue-resident macrophages involved in phagocytosis and immune regulation. Eosinophils arise from myeloid progenitor cells in the bone marrow and play key roles in combating parasitic infections and modulating allergic inflammatory responses. Understanding the distinct hematopoietic lineages and cellular differentiation pathways highlights the specialized functions of macrophages and eosinophils in immune defense mechanisms.
Key Roles in Inflammation and Immunity
Macrophagic cells play a critical role in inflammation and immunity by phagocytosing pathogens, presenting antigens, and secreting cytokines that orchestrate the immune response. Eosinophilic cells are primarily involved in combating parasitic infections and modulating allergic inflammation through the release of cytotoxic granules and inflammatory mediators. Both cell types contribute to immune regulation but differ in target specificity and effector functions within the inflammatory microenvironment.
Common Disorders Associated with Macrophages
Macrophages play a crucial role in chronic inflammatory disorders such as tuberculosis, atherosclerosis, and rheumatoid arthritis due to their ability to phagocytose pathogens and debris while secreting pro-inflammatory cytokines. Unlike eosinophils, which primarily combat parasitic infections and mediate allergic responses, macrophages are involved in tissue remodeling and immune regulation in diseases like sarcoidosis and chronic obstructive pulmonary disease (COPD). The pathological accumulation and activation of macrophages contribute to granuloma formation and sustained inflammation in these disorders.
Diseases Linked to Eosinophil Overactivity
Diseases linked to eosinophil overactivity include eosinophilic esophagitis, asthma, and hypereosinophilic syndrome, where excessive eosinophil accumulation leads to tissue inflammation and damage. Macrophagic activity, in contrast, is primarily associated with chronic inflammation and pathogen clearance but does not typically cause the same degree of tissue eosinophilia. Understanding the distinct roles of eosinophils and macrophages is crucial for diagnosing and targeting treatments in eosinophil-driven disorders.
Diagnostic Differences: Identifying Cell Types
Macrophagic and eosinophilic cells differ significantly in diagnostic pathology based on their morphology and staining properties; macrophages exhibit large, irregular shapes with abundant cytoplasm and are identified using CD68 immunostaining, while eosinophils are characterized by bilobed nuclei and prominent eosinophilic granules, detectable with eosin dye or by their expression of granule proteins like eosinophil peroxidase. Flow cytometry and immunohistochemistry facilitate precise differentiation, with macrophages showing markers such as CD14 and CD163, whereas eosinophils express Siglec-8 and CCR3. Accurate identification of these cells aids in diagnosing various inflammatory and immune-mediated diseases by correlating cell presence with specific pathological contexts.
Therapeutic Approaches Targeting Macrophages and Eosinophils
Therapeutic approaches targeting macrophages often involve modulating their polarization states, using agents like CSF-1R inhibitors to reduce pro-inflammatory M1 macrophages and promote tissue repair by enhancing M2 macrophages. In contrast, treatments aimed at eosinophils primarily utilize monoclonal antibodies such as mepolizumab and benralizumab that target IL-5 or its receptor, leading to eosinophil depletion and reduced inflammation in diseases like asthma and eosinophilic esophagitis. Emerging strategies explore combined modulation of macrophage and eosinophil activity to achieve synergistic effects in chronic inflammatory and allergic disorders.
Conclusion: Clinical Implications and Future Directions
Macrophagic inflammation is primarily associated with chronic tissue damage and repair processes, influencing the progression of diseases such as tuberculosis and atherosclerosis, while eosinophilic responses are linked to allergic reactions and parasitic infections, playing critical roles in asthma and eosinophilic esophagitis management. Understanding the distinct cellular pathways and cytokine profiles underlying macrophagic versus eosinophilic inflammation enables the development of targeted therapies, including anti-inflammatory agents and immunomodulators tailored to specific disease mechanisms. Future research should emphasize biomarker identification for precise diagnosis and personalized treatment strategies to optimize clinical outcomes in inflammatory and immune-mediated disorders.
Macrophagic Infographic
 libterm.com
libterm.com