Stenosis narrows blood vessels, restricting blood flow and increasing the risk of complications like heart attacks or strokes, while an aneurysm involves a weakened vessel wall that can bulge and potentially rupture, posing serious health threats. Understanding the differences in causes, symptoms, and treatments between stenosis and aneurysm is crucial for timely medical intervention. Discover more about how these vascular conditions impact your health and what steps you can take to manage them in the rest of this article.
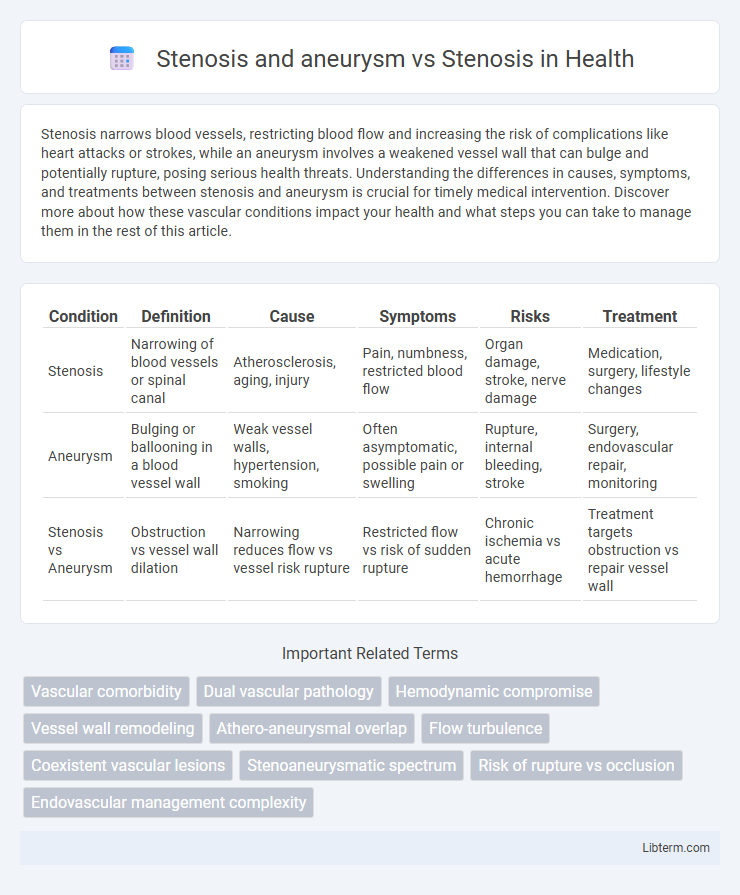
Table of Comparison
| Condition | Definition | Cause | Symptoms | Risks | Treatment |
|---|---|---|---|---|---|
| Stenosis | Narrowing of blood vessels or spinal canal | Atherosclerosis, aging, injury | Pain, numbness, restricted blood flow | Organ damage, stroke, nerve damage | Medication, surgery, lifestyle changes |
| Aneurysm | Bulging or ballooning in a blood vessel wall | Weak vessel walls, hypertension, smoking | Often asymptomatic, possible pain or swelling | Rupture, internal bleeding, stroke | Surgery, endovascular repair, monitoring |
| Stenosis vs Aneurysm | Obstruction vs vessel wall dilation | Narrowing reduces flow vs vessel risk rupture | Restricted flow vs risk of sudden rupture | Chronic ischemia vs acute hemorrhage | Treatment targets obstruction vs repair vessel wall |
Introduction to Stenosis and Aneurysm
Stenosis refers to the abnormal narrowing of blood vessels or other tubular structures in the body, often leading to restricted blood flow and increased pressure. Aneurysm, on the other hand, involves the abnormal bulging or ballooning of a weakened blood vessel wall, which poses a risk of rupture and severe bleeding. Both conditions affect vascular health but differ in pathology, with stenosis causing obstruction and aneurysm risking vessel rupture.
Defining Stenosis: Causes and Types
Stenosis refers to the abnormal narrowing of blood vessels or other tubular structures, often caused by factors such as atherosclerosis, inflammation, or congenital defects. It can be categorized into several types based on location, including arterial stenosis, spinal stenosis, and valvular stenosis, each presenting unique clinical implications. Unlike aneurysm, which involves vessel dilation, stenosis primarily restricts blood flow, leading to ischemia and organ dysfunction.
Understanding Aneurysms: Causes and Risks
Understanding aneurysms involves recognizing abnormal bulges in blood vessel walls caused by factors such as high blood pressure, atherosclerosis, or genetic predisposition. Unlike stenosis, which is the narrowing of blood vessels impairing blood flow, aneurysms pose a risk of rupture, leading to life-threatening bleeding. Early detection through imaging techniques and management of risk factors are critical for preventing aneurysm complications.
Stenosis vs. Aneurysm: Key Differences
Stenosis and aneurysm represent two distinct vascular conditions with opposite effects on blood vessels: stenosis involves abnormal narrowing that restricts blood flow, while aneurysm denotes a localized vessel wall dilation that increases rupture risk. Key differences revolve around pathophysiology--stenosis results from plaque buildup or vessel wall thickening, leading to ischemia, whereas aneurysms arise from vessel wall weakening causing bulging. Clinically, stenosis primarily causes symptoms of obstruction such as angina or claudication, contrasted by aneurysm risks of hemorrhage or embolism, necessitating tailored diagnostic and treatment approaches.
Combined Stenosis and Aneurysm: Clinical Implications
Combined stenosis and aneurysm significantly elevate the risk of vascular complications due to simultaneous arterial narrowing and dilation, disrupting hemodynamic stability. This dual pathology increases the likelihood of thromboembolic events, vessel rupture, and subsequent ischemic damage compared to isolated stenosis. Clinical management requires precise imaging techniques and tailored treatment strategies to address the complex interplay of vessel obstruction and wall weakening.
Symptoms of Stenosis and Aneurysm
Stenosis commonly causes symptoms such as chest pain, shortness of breath, fatigue, and dizziness due to restricted blood flow through narrowed arteries or heart valves. Aneurysms may remain asymptomatic until they enlarge or rupture, but when symptoms occur, they include severe localized pain, pulsating masses, or neurological deficits depending on the aneurysm's location. Differentiating symptoms is crucial for diagnosis, as stenosis involves blood flow obstruction while aneurysms involve vessel wall dilation and potential rupture risks.
Diagnostic Approaches: Stenosis Alone vs. With Aneurysm
Diagnostic approaches for stenosis alone primarily utilize Doppler ultrasound and angiography to assess vessel narrowing and blood flow restriction. When stenosis occurs with an aneurysm, advanced imaging techniques such as computed tomography angiography (CTA) and magnetic resonance angiography (MRA) are preferred to simultaneously evaluate vessel wall integrity, aneurysm size, and stenotic severity. The presence of an aneurysm necessitates detailed hemodynamic assessment to guide appropriate interventional or surgical management, as standard stenosis evaluation methods may not fully capture the complexity of combined pathology.
Treatment Strategies: Stenosis vs. Stenosis with Aneurysm
Treatment strategies for stenosis primarily involve angioplasty and stent placement to restore blood flow by widening narrowed vessels. When stenosis coexists with an aneurysm, management becomes more complex, often requiring combined endovascular techniques to address both vessel narrowing and aneurysm stabilization, such as stent grafting or coil embolization. Careful imaging assessment guides therapeutic decisions, prioritizing the prevention of aneurysm rupture alongside maintaining vessel patency.
Prognosis and Complications
Stenosis involves the narrowing of blood vessels, leading to reduced blood flow and increased risk of ischemia, while aneurysms cause vessel wall dilation, risking rupture and hemorrhage. Prognosis for stenosis depends on the severity and location, with risks including thrombosis and organ damage, whereas aneurysms carry a higher risk of sudden life-threatening complications like rupture and stroke. Both conditions require vigilant monitoring and management to prevent serious cardiovascular events and improve patient outcomes.
Prevention and Patient Management
Prevention of both stenosis and aneurysm involves controlling risk factors like hypertension, smoking, and high cholesterol through lifestyle changes and medication management. In patient management, regular imaging such as ultrasound or CT scans is essential to monitor disease progression, with stenosis often treated by angioplasty or stenting to restore blood flow, whereas aneurysms may require surgical repair or endovascular procedures to prevent rupture. Coordinated care including blood pressure control, antiplatelet therapy, and lifestyle modifications significantly reduces complications in both conditions.
Stenosis and aneurysm Infographic
 libterm.com
libterm.com