Orthotopic refers to the implantation or natural occurrence of cells, tissues, or organs in their original anatomical position, crucial in medical and biological contexts such as cancer research or organ transplants. This approach enhances the relevance of experimental models by closely mimicking human physiological conditions, improving treatment outcomes and disease understanding. Explore the rest of the article to discover how orthotopic techniques impact cutting-edge therapies and research developments.
Table of Comparison
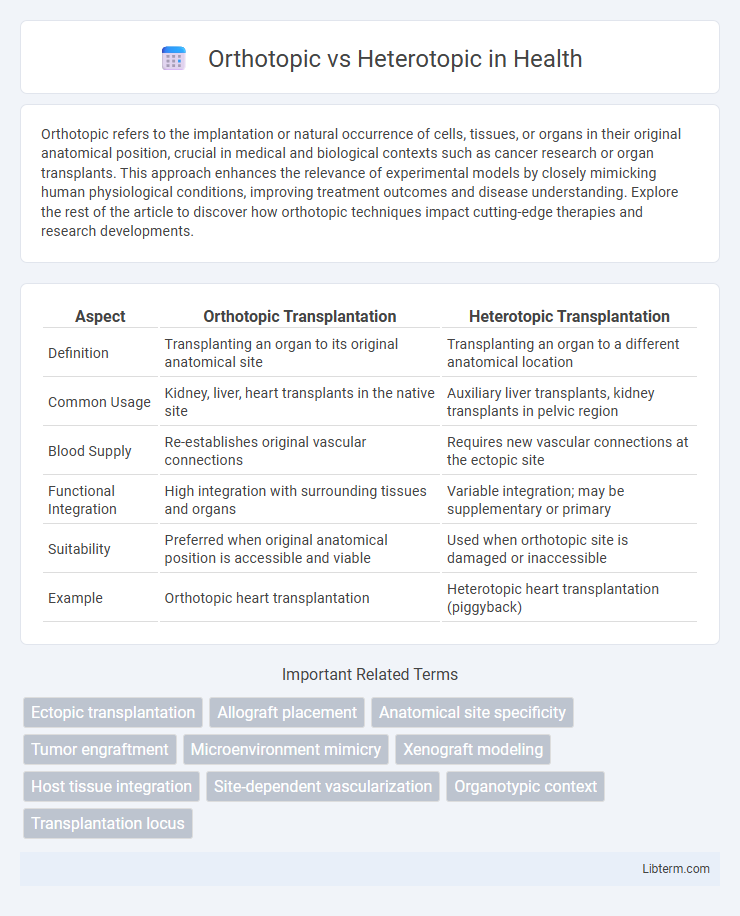
| Aspect | Orthotopic Transplantation | Heterotopic Transplantation |
|---|---|---|
| Definition | Transplanting an organ to its original anatomical site | Transplanting an organ to a different anatomical location |
| Common Usage | Kidney, liver, heart transplants in the native site | Auxiliary liver transplants, kidney transplants in pelvic region |
| Blood Supply | Re-establishes original vascular connections | Requires new vascular connections at the ectopic site |
| Functional Integration | High integration with surrounding tissues and organs | Variable integration; may be supplementary or primary |
| Suitability | Preferred when original anatomical position is accessible and viable | Used when orthotopic site is damaged or inaccessible |
| Example | Orthotopic heart transplantation | Heterotopic heart transplantation (piggyback) |
Introduction to Orthotopic and Heterotopic Models
Orthotopic models involve implanting cells or tissues into the original, anatomically correct location within the host organism, closely mimicking the natural tumor microenvironment and disease progression. Heterotopic models, typically using subcutaneous implantation, provide easier monitoring and access but lack the precise microenvironmental cues of the tissue of origin. Both models are essential in preclinical research to evaluate therapeutic responses and tumor biology, with orthotopic models offering more clinically relevant data.
Defining Orthotopic Implantation
Orthotopic implantation involves placing tissue or cells into the original, anatomically correct location within the body, ensuring a natural microenvironment that supports proper function and integration. This method is commonly used in cancer research and organ transplantation to replicate physiological conditions more accurately than heterotopic implantation, where tissues are placed in non-native sites. Orthotopic models improve the relevance of experimental results by mimicking the native tissue environment and interactions critical for disease progression and therapeutic response.
Understanding Heterotopic Implantation
Heterotopic implantation refers to the transplantation of tissue or organs into a different anatomical location than the original site, commonly used in experimental and clinical settings to study graft function and immune response. Unlike orthotopic implantation, which involves placement in the native anatomical site, heterotopic implants allow for easier access, monitoring, and potential immunological isolation. This approach is frequently employed in cardiac and kidney transplant research to assess vascularization, viability, and functional integration outside the orthotopic environment.
Key Differences Between Orthotopic and Heterotopic Approaches
Orthotopic transplantation involves placing the organ or tissue in its original anatomical location, preserving natural physiological conditions and vascular connections, whereas heterotopic transplantation implants the organ in a different site, often to provide supplemental function without removing the native organ. Orthotopic approaches typically result in better functional integration and immune tolerance, while heterotopic methods offer surgical flexibility and are valuable in cases where the original site is compromised. Key differences also include surgical complexity, graft survival rates, and post-transplant monitoring requirements, with orthotopic procedures generally requiring more precise anatomical alignment.
Advantages of Orthotopic Models
Orthotopic models offer significant advantages by closely mimicking the natural tumor microenvironment, which enhances the accuracy of cancer progression and metastasis studies. These models allow for more precise evaluation of therapeutic responses due to the tumor's original anatomical context, facilitating better prediction of clinical outcomes. The preservation of tumor-stroma interactions in orthotopic implants ensures relevant insights into tumor biology and treatment resistance mechanisms, making them superior to heterotopic models.
Advantages of Heterotopic Models
Heterotopic models offer the advantage of easier surgical implantation and monitoring due to their superficial and accessible locations, which simplifies tumor growth assessment. These models provide consistent and reproducible tumor microenvironments, facilitating controlled studies of tumor biology and therapeutic responses. Enhanced accessibility in heterotopic models enables frequent sampling and imaging, optimizing evaluation of treatment efficacy and disease progression.
Applications in Cancer Research
Orthotopic tumor models, where cancer cells are implanted into the original organ site, provide a more accurate tumor microenvironment and metastatic pattern, enhancing the study of tumor behavior and drug response in cancer research. Heterotopic models, typically involving subcutaneous implantation, offer easier tumor monitoring and high-throughput drug screening but lack the organ-specific interactions critical for metastasis studies. Utilizing both orthotopic and heterotopic models allows researchers to balance physiological relevance and experimental efficiency when evaluating novel cancer therapies.
Limitations and Challenges
Orthotopic transplantation faces challenges such as complex surgical procedures and higher risk of graft rejection due to the delicate anatomical site. Heterotopic transplantation encounters limitations including impaired functionality and integration as the graft is placed in a non-native location, leading to suboptimal physiological outcomes. Both methods require meticulous immunosuppressive management to prevent rejection, yet differ significantly in surgical complexity and post-operative recovery demands.
Selecting the Appropriate Model
Selecting the appropriate model between orthotopic and heterotopic transplantation depends on the research objectives and tumor microenvironment relevance. Orthotopic models involve implanting cells or tissues into the organ of origin, closely mimicking tumor growth, metastasis, and drug response in a native context. Heterotopic models, typically subcutaneous, offer easier tumor monitoring and quicker growth assessment but may lack the specific interactions present in the original tissue site.
Future Trends in Orthotopic and Heterotopic Research
Future trends in orthotopic and heterotopic research emphasize advancements in tissue engineering and regenerative medicine, with a focus on enhancing graft integration and function. Innovations in biomaterials and 3D bioprinting are driving personalized therapies, improving outcomes in organ transplantation and repair. Ongoing studies explore immune modulation techniques to minimize rejection and extend graft longevity in both orthotopic and heterotopic contexts.
Orthotopic Infographic
 libterm.com
libterm.com