Respiratory failure occurs when the lungs cannot adequately exchange oxygen and carbon dioxide, leading to insufficient oxygen supply or elevated carbon dioxide levels in the blood. This condition can result from various causes, including chronic lung diseases, infections, or trauma, and often requires immediate medical intervention. Discover how understanding the symptoms, types, and treatments of respiratory failure can help you recognize its urgency and explore effective management strategies in the full article.
Table of Comparison
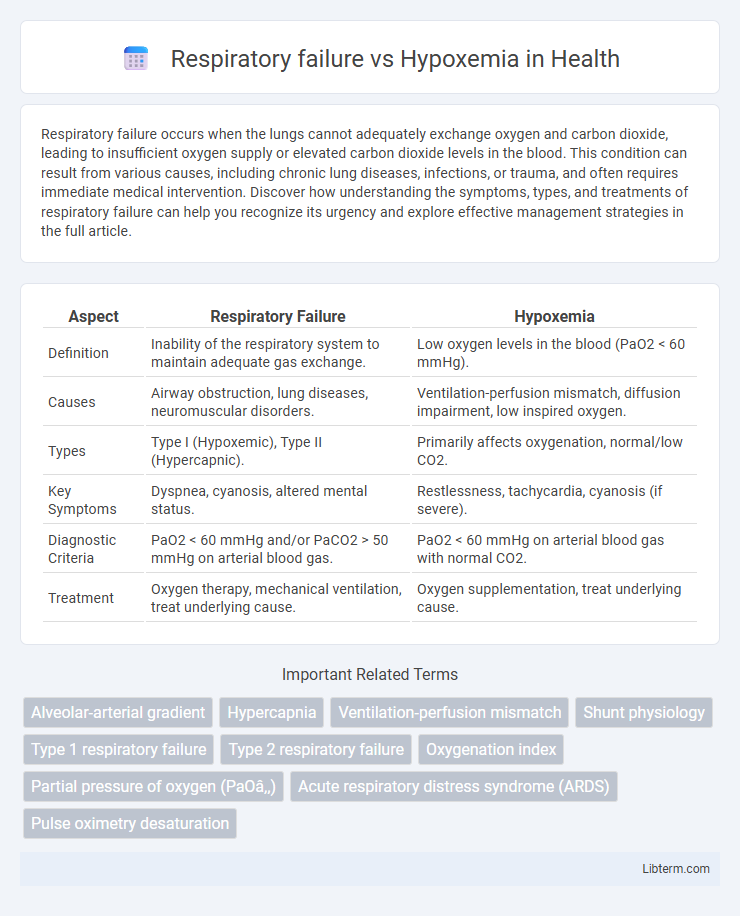
| Aspect | Respiratory Failure | Hypoxemia |
|---|---|---|
| Definition | Inability of the respiratory system to maintain adequate gas exchange. | Low oxygen levels in the blood (PaO2 < 60 mmHg). |
| Causes | Airway obstruction, lung diseases, neuromuscular disorders. | Ventilation-perfusion mismatch, diffusion impairment, low inspired oxygen. |
| Types | Type I (Hypoxemic), Type II (Hypercapnic). | Primarily affects oxygenation, normal/low CO2. |
| Key Symptoms | Dyspnea, cyanosis, altered mental status. | Restlessness, tachycardia, cyanosis (if severe). |
| Diagnostic Criteria | PaO2 < 60 mmHg and/or PaCO2 > 50 mmHg on arterial blood gas. | PaO2 < 60 mmHg on arterial blood gas with normal CO2. |
| Treatment | Oxygen therapy, mechanical ventilation, treat underlying cause. | Oxygen supplementation, treat underlying cause. |
Introduction to Respiratory Failure and Hypoxemia
Respiratory failure is a clinical condition characterized by the inability of the respiratory system to maintain adequate gas exchange, resulting in insufficient oxygenation or carbon dioxide elimination. Hypoxemia specifically refers to low oxygen levels in the blood, which can occur independently or as a component of respiratory failure. Understanding the distinction between hypoxemia as a measurable reduction in arterial oxygen tension and respiratory failure as a broader dysfunction of respiratory mechanics is essential for accurate diagnosis and management.
Defining Respiratory Failure
Respiratory failure occurs when the respiratory system cannot maintain adequate gas exchange, leading to insufficient oxygenation or carbon dioxide elimination. It encompasses two types: hypoxemic respiratory failure, characterized by low arterial oxygen levels (PaO2 < 60 mmHg), and hypercapnic respiratory failure, marked by elevated arterial carbon dioxide levels (PaCO2 > 50 mmHg). Hypoxemia specifically refers to low oxygen levels in the blood and can be a component of respiratory failure but does not alone define the condition.
Understanding Hypoxemia
Hypoxemia refers to abnormally low levels of oxygen in the arterial blood, typically measured by a partial pressure of oxygen (PaO2) below 80 mm Hg or oxygen saturation (SpO2) under 90%. It is a critical component of respiratory failure but can occur independently due to factors like ventilation-perfusion mismatch, diffusion impairment, or low inspired oxygen. Accurate diagnosis of hypoxemia guides targeted treatment strategies such as supplemental oxygen or mechanical ventilation to restore adequate tissue oxygenation.
Key Differences Between Respiratory Failure and Hypoxemia
Respiratory failure occurs when the respiratory system fails to maintain adequate gas exchange, resulting in abnormal levels of oxygen (hypoxemia) or carbon dioxide (hypercapnia) in the blood, while hypoxemia specifically refers to low oxygen levels in the blood regardless of carbon dioxide status. Respiratory failure is classified into type 1 (hypoxemic) characterized by PaO2 less than 60 mmHg with normal or low PaCO2, and type 2 (hypercapnic) defined by elevated PaCO2 above 50 mmHg, whereas hypoxemia can exist independently in conditions like altitude sickness or pulmonary embolism. The clinical management of respiratory failure often involves ventilatory support and treating underlying causes, whereas hypoxemia treatment focuses primarily on oxygen supplementation and improving oxygen delivery.
Causes of Respiratory Failure
Respiratory failure results from conditions impairing gas exchange or ventilation, including chronic obstructive pulmonary disease (COPD), acute respiratory distress syndrome (ARDS), pneumonia, pulmonary embolism, and neuromuscular disorders like Guillain-Barre syndrome. Unlike hypoxemia, which specifically denotes low arterial oxygen levels, respiratory failure encompasses both hypoxemic (type I) and hypercapnic (type II) failure caused by ventilation-perfusion mismatch or respiratory muscle fatigue. Understanding these causes aids in differentiating respiratory failure from isolated hypoxemia and guides appropriate clinical management.
Causes of Hypoxemia
Hypoxemia primarily results from impaired oxygen exchange due to conditions such as ventilation-perfusion (V/Q) mismatch, diffusion impairment, hypoventilation, and shunting within the lungs. Common causes include chronic obstructive pulmonary disease (COPD), pneumonia, pulmonary embolism, and acute respiratory distress syndrome (ARDS). Hypoxemia differs from respiratory failure, which encompasses inadequate ventilation leading to both hypoxemia and hypercapnia.
Clinical Presentation and Symptoms
Respiratory failure presents with severe dyspnea, altered mental status, and cyanosis due to inadequate gas exchange, often accompanied by hypercapnia and hypoxemia. Hypoxemia primarily manifests as confusion, tachypnea, and cyanosis, reflecting decreased arterial oxygen levels without necessarily elevated carbon dioxide. Both conditions require prompt clinical assessment but differ as respiratory failure includes ventilatory pump dysfunction, whereas hypoxemia strictly refers to low blood oxygen concentration.
Diagnostic Approaches
Diagnosing respiratory failure involves arterial blood gas (ABG) analysis to assess levels of oxygen (PaO2) and carbon dioxide (PaCO2), identifying impaired gas exchange or ventilation. Hypoxemia diagnosis specifically relies on measuring arterial oxygen saturation (SaO2) and partial pressure of oxygen (PaO2) to confirm decreased oxygen levels in the blood. Imaging studies such as chest X-rays and pulmonary function tests can further aid in differentiating the underlying causes of respiratory failure and hypoxemia.
Treatment and Management Strategies
Respiratory failure often requires mechanical ventilation and oxygen therapy tailored to the underlying cause, such as bronchodilators for obstructive lung disease or antibiotics for infections. Hypoxemia treatment prioritizes supplemental oxygen delivery, with methods including nasal cannula, non-rebreather masks, or high-flow oxygen systems, depending on severity. Both conditions benefit from continuous monitoring of arterial blood gases and close management in intensive care settings for optimal outcomes.
Prognosis and Outcomes
Respiratory failure often presents with severe hypoxemia and hypercapnia, leading to a higher risk of mortality and long-term morbidity compared to isolated hypoxemia. Prognosis depends on underlying etiology, severity, and promptness of intervention, with respiratory failure requiring mechanical ventilation and intensive care. Outcomes in hypoxemia without respiratory failure tend to be more favorable, particularly when corrected early, minimizing organ damage and improving survival rates.
Respiratory failure Infographic
 libterm.com
libterm.com