Hypercalcemia occurs when calcium levels in the blood rise above normal, potentially causing symptoms like fatigue, nausea, and confusion. Identifying the underlying cause is crucial to effectively manage this condition and prevent complications such as kidney stones or bone pain. Explore the rest of the article to understand the causes, symptoms, and treatment options for hypercalcemia.
Table of Comparison
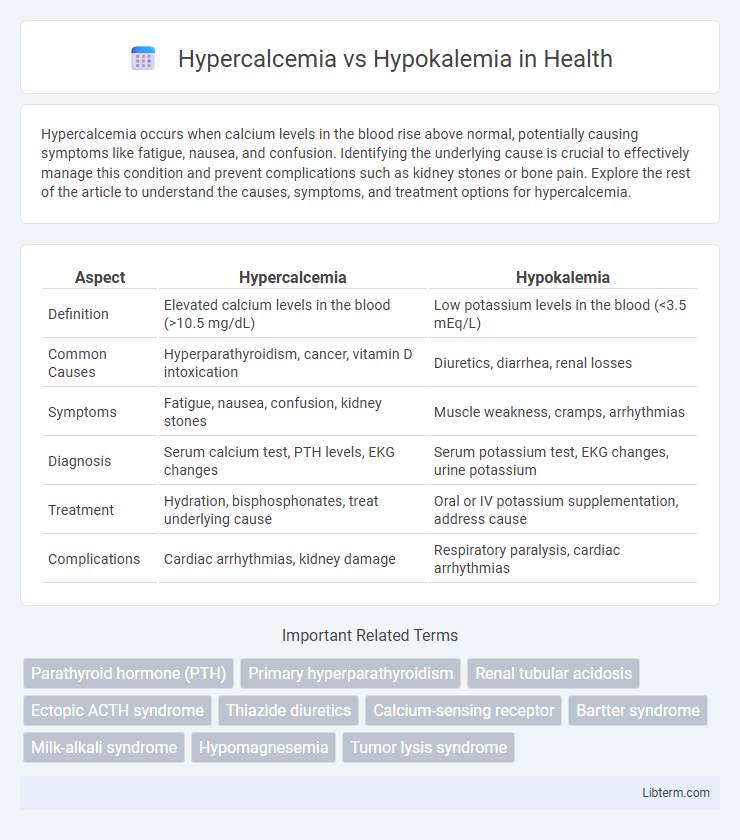
| Aspect | Hypercalcemia | Hypokalemia |
|---|---|---|
| Definition | Elevated calcium levels in the blood (>10.5 mg/dL) | Low potassium levels in the blood (<3.5 mEq/L) |
| Common Causes | Hyperparathyroidism, cancer, vitamin D intoxication | Diuretics, diarrhea, renal losses |
| Symptoms | Fatigue, nausea, confusion, kidney stones | Muscle weakness, cramps, arrhythmias |
| Diagnosis | Serum calcium test, PTH levels, EKG changes | Serum potassium test, EKG changes, urine potassium |
| Treatment | Hydration, bisphosphonates, treat underlying cause | Oral or IV potassium supplementation, address cause |
| Complications | Cardiac arrhythmias, kidney damage | Respiratory paralysis, cardiac arrhythmias |
Understanding Hypercalcemia and Hypokalemia
Hypercalcemia is characterized by elevated calcium levels in the blood, often caused by hyperparathyroidism, malignancies, or excessive vitamin D intake, leading to symptoms like fatigue, nausea, and kidney stones. Hypokalemia refers to low potassium levels, commonly resulting from diuretic use, vomiting, or diarrhea, and can cause muscle weakness, arrhythmias, and cramps. Accurate diagnosis involves serum electrolyte tests, with treatment targeting underlying causes and restoring electrolyte balance to prevent severe complications.
Key Differences Between Hypercalcemia and Hypokalemia
Hypercalcemia is characterized by elevated calcium levels in the blood, typically above 10.5 mg/dL, whereas hypokalemia involves low potassium levels, usually below 3.5 mEq/L. Symptoms of hypercalcemia include fatigue, nausea, and kidney stones, while hypokalemia often presents with muscle weakness, cramps, and cardiac arrhythmias. Treatment strategies differ significantly, targeting calcium reduction through hydration and bisphosphonates in hypercalcemia, and potassium supplementation in hypokalemia to restore electrolyte balance.
Causes of Hypercalcemia
Hypercalcemia primarily results from hyperparathyroidism, malignancies such as multiple myeloma and metastatic cancers, and excessive vitamin D intake, leading to elevated serum calcium levels. Other causes include prolonged immobilization, thiazide diuretics use, and granulomatous diseases like sarcoidosis that increase calcium absorption or bone resorption. Unlike hypokalemia, which stems from potassium loss or shifts, hypercalcemia's causes involve altered calcium metabolism and cellular regulation.
Causes of Hypokalemia
Hypokalemia, characterized by low serum potassium levels below 3.5 mEq/L, commonly results from excessive potassium loss due to diuretic use, chronic kidney disease, or gastrointestinal disturbances like diarrhea and vomiting. Other causes include hyperaldosteronism, which increases renal potassium excretion, and certain medications such as amphotericin B or corticosteroids. Understanding these etiologies is crucial for differentiating hypokalemia from hypercalcemia, where elevated calcium levels often arise from hyperparathyroidism or malignancy.
Signs and Symptoms of Hypercalcemia
Hypercalcemia primarily presents with symptoms such as excessive thirst, frequent urination, abdominal pain, nausea, vomiting, and muscle weakness. Neurological signs include confusion, lethargy, and in severe cases, coma, while cardiac manifestations often involve arrhythmias and short QT interval on ECG. Unlike hypokalemia, which causes muscle cramps and arrhythmias due to low potassium, hypercalcemia's hallmark features stem from elevated calcium levels affecting kidney function, neuromuscular activity, and cardiac conduction.
Signs and Symptoms of Hypokalemia
Hypokalemia presents with muscle weakness, fatigue, and cramping due to low potassium levels disrupting cellular function and nerve conduction. Patients may experience palpitations, arrhythmias, and in severe cases, paralysis or respiratory failure. Hypokalemia often causes constipation and polyuria as potassium imbalance affects smooth muscle contraction and kidney function.
Diagnostic Approaches for Hypercalcemia vs Hypokalemia
Diagnostic approaches for hypercalcemia involve measuring serum calcium levels, assessing parathyroid hormone (PTH) concentrations to differentiate primary hyperparathyroidism from malignancy-related causes, and conducting imaging studies like neck ultrasound or sestamibi scans for parathyroid adenomas. In contrast, hypokalemia diagnosis centers on serum potassium measurement, evaluating urinary potassium excretion to distinguish renal from extrarenal losses, and assessing acid-base status to identify underlying metabolic or renal tubular disorders. Both conditions require comprehensive biochemical panels and clinical correlation to guide targeted treatment strategies effectively.
Treatment Strategies for Hypercalcemia
Treatment strategies for hypercalcemia primarily focus on reducing serum calcium levels through intravenous hydration with normal saline to promote renal calcium excretion. Bisphosphonates such as pamidronate or zoledronic acid are commonly administered to inhibit osteoclast-mediated bone resorption, particularly in malignancy-associated hypercalcemia. Calcitonin offers a rapid but short-term reduction in calcium levels, while corticosteroids are effective in hypercalcemia due to vitamin D intoxication or granulomatous diseases.
Treatment Strategies for Hypokalemia
Treatment strategies for hypokalemia focus on restoring potassium levels through oral or intravenous potassium supplementation, depending on severity. Identifying and addressing underlying causes such as diuretic use, gastrointestinal losses, or magnesium deficiency is crucial for effective management. Continuous monitoring of serum potassium and cardiac function helps prevent complications associated with persistent hypokalemia.
Preventive Measures and Prognosis
Preventive measures for hypercalcemia include maintaining adequate hydration, avoiding excessive calcium or vitamin D intake, and regular monitoring of serum calcium levels, especially in patients with risk factors like hyperparathyroidism or malignancies. For hypokalemia, prevention involves ensuring sufficient dietary potassium intake, managing medications that affect potassium levels, and monitoring electrolyte balance in conditions like diuretic use or gastrointestinal losses. Prognosis for hypercalcemia depends on the underlying cause, with benign cases resolving upon treatment, while severe or chronic hypercalcemia may lead to renal impairment or cardiac issues; hypokalemia prognosis is generally favorable with prompt correction but can result in serious arrhythmias or muscle weakness if untreated.
Hypercalcemia Infographic
 libterm.com
libterm.com