Anesthesia is a critical medical practice that ensures you remain pain-free and unconscious during surgical procedures, utilizing medications tailored to your specific needs. Understanding the types, risks, and recovery aspects can help alleviate concerns and improve your overall surgical experience. Explore the rest of the article to learn more about how anesthesia works and what to expect before, during, and after your procedure.
Table of Comparison
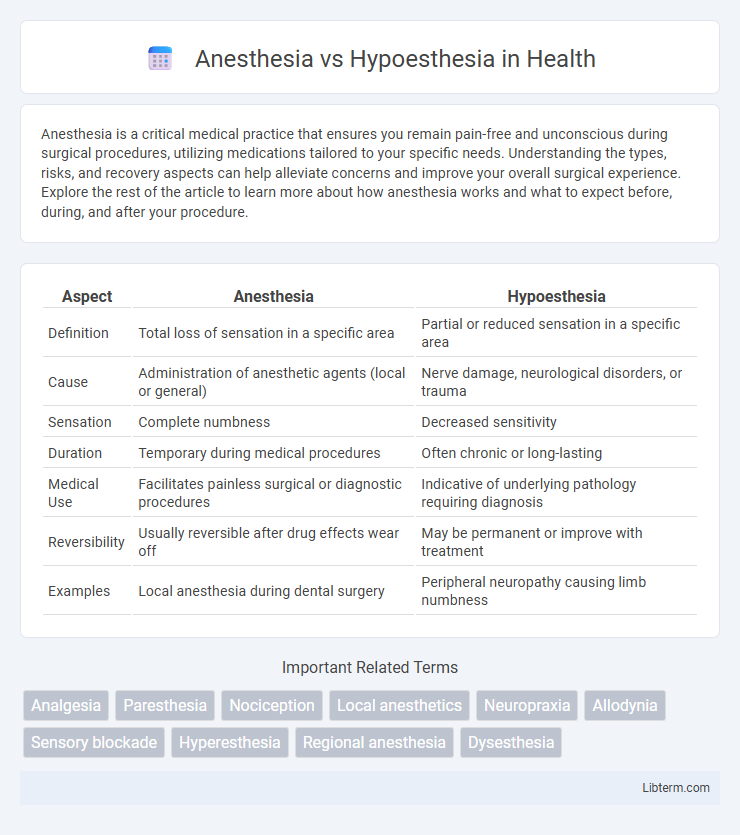
| Aspect | Anesthesia | Hypoesthesia |
|---|---|---|
| Definition | Total loss of sensation in a specific area | Partial or reduced sensation in a specific area |
| Cause | Administration of anesthetic agents (local or general) | Nerve damage, neurological disorders, or trauma |
| Sensation | Complete numbness | Decreased sensitivity |
| Duration | Temporary during medical procedures | Often chronic or long-lasting |
| Medical Use | Facilitates painless surgical or diagnostic procedures | Indicative of underlying pathology requiring diagnosis |
| Reversibility | Usually reversible after drug effects wear off | May be permanent or improve with treatment |
| Examples | Local anesthesia during dental surgery | Peripheral neuropathy causing limb numbness |
Introduction to Anesthesia and Hypoesthesia
Anesthesia refers to the medically induced loss of sensation, typically used to prevent pain during surgical procedures, involving agents that block nerve signals to the brain. Hypoesthesia is characterized by a diminished sensitivity to sensory stimuli, often resulting from nerve damage or neurological disorders, leading to partial numbness or reduced sensation. Understanding the distinct mechanisms and clinical applications of anesthesia and hypoesthesia is essential in diagnosing sensory impairments and managing patient care effectively.
Defining Anesthesia: Meaning and Mechanism
Anesthesia is a medically induced state of controlled, temporary loss of sensation or awareness, primarily used to prevent pain during surgical procedures. Its mechanism involves interrupting nerve signal transmission to the brain by using anesthetic agents that block synaptic activity or sodium channels in nerve cells. This controlled inhibition of nerve conduction differentiates anesthesia from hypoesthesia, which is a partial loss or reduction of sensation.
Understanding Hypoesthesia: Symptoms and Causes
Hypoesthesia refers to a reduced sense of touch or sensation, often caused by nerve damage, diabetes, or neurological disorders. Symptoms include numbness, tingling, and a decreased ability to feel pain or temperature changes, which can affect specific body areas depending on the underlying condition. Accurate diagnosis of hypoesthesia involves neurological exams and imaging tests to identify the extent and cause of sensory impairment, guiding effective treatment plans.
Key Differences Between Anesthesia and Hypoesthesia
Anesthesia refers to a medically induced, temporary loss of sensation or awareness, often used during surgical procedures to prevent pain, while hypoesthesia is a reduced sensitivity to sensory stimuli, typically resulting from nerve damage or neurological conditions. Anesthesia usually involves a controlled and reversible state administered by healthcare professionals, whereas hypoesthesia is an abnormal condition that may persist and requires diagnosis and treatment of the underlying cause. The key difference lies in anesthesia's intentional and complete sensory blockade compared to the partial and often pathological sensory diminution seen in hypoesthesia.
Clinical Applications of Anesthesia
Anesthesia involves the controlled and reversible loss of sensation, utilized extensively in surgical procedures to prevent pain and discomfort, ensuring patient immobility and safety. Its clinical applications span general anesthesia for major surgeries, regional anesthesia like epidurals for childbirth and limb surgeries, and local anesthesia for minor outpatient procedures. Advances in anesthesia techniques and pharmacology enhance precise dosing, rapid recovery, and minimize adverse effects, improving patient outcomes in diverse medical interventions.
Common Causes and Types of Hypoesthesia
Anesthesia is the complete loss of sensation, often induced medically for surgical procedures, while hypoesthesia refers to a partial reduction in sensory perception. Common causes of hypoesthesia include nerve compression, diabetes mellitus, multiple sclerosis, and peripheral neuropathy. Types of hypoesthesia vary based on location and underlying pathology, such as focal hypoesthesia from localized nerve injury or generalized hypoesthesia associated with systemic conditions.
Diagnostic Approaches: Anesthesia vs Hypoesthesia
Diagnostic approaches for anesthesia and hypoesthesia involve clinical sensory testing to assess the extent and type of nerve impairment. Anesthesia is characterized by complete loss of sensation, typically evaluated through pinprick, temperature, and light touch tests, while hypoesthesia presents as partial sensory loss, requiring quantitative sensory testing to measure reduced sensitivity thresholds. Advanced imaging techniques, such as MRI or nerve conduction studies, support differential diagnosis by revealing underlying nerve or central nervous system abnormalities.
Risks and Complications Associated with Each Condition
Anesthesia involves complete loss of sensation, posing risks such as respiratory depression, cardiovascular instability, and allergic reactions, while hypoesthesia denotes partial sensory reduction, which may lead to nerve damage or persistent numbness. Complications from anesthesia can include postoperative cognitive dysfunction and infection at the injection site, whereas hypoesthesia risks involve improper nerve healing and chronic pain syndromes. Careful monitoring and tailored management strategies are essential to minimize adverse outcomes in both conditions.
Treatment Options and Management Strategies
Anesthesia typically requires treatment through regional or general anesthetics tailored to surgical procedures, emphasizing precise dosage control to ensure patient safety and efficacy. Hypoesthesia management involves addressing underlying causes such as nerve compression or systemic conditions via physical therapy, medications like analgesics or corticosteroids, and sometimes surgical intervention to restore normal sensation. Both conditions benefit from ongoing monitoring and multimodal approaches to optimize recovery and minimize complications.
Conclusion: Choosing the Right Approach for Patient Care
Selecting the appropriate approach between anesthesia and hypoesthesia hinges on the specific clinical scenario and desired patient outcome. Anesthesia provides complete loss of sensation, ideal for surgical interventions requiring pain-free conditions, while hypoesthesia involves partial sensory reduction suited for less invasive procedures or diagnostic purposes. Tailoring the choice to patient needs and procedural requirements ensures optimal pain management and safety during medical care.
Anesthesia Infographic
 libterm.com
libterm.com