Pyuria, characterized by the presence of white blood cells in the urine, often signals an underlying urinary tract infection or inflammation. Accurate diagnosis and timely treatment are essential to prevent complications and restore urinary health effectively. Explore this article to learn more about the causes, symptoms, and management of pyuria for Your well-being.
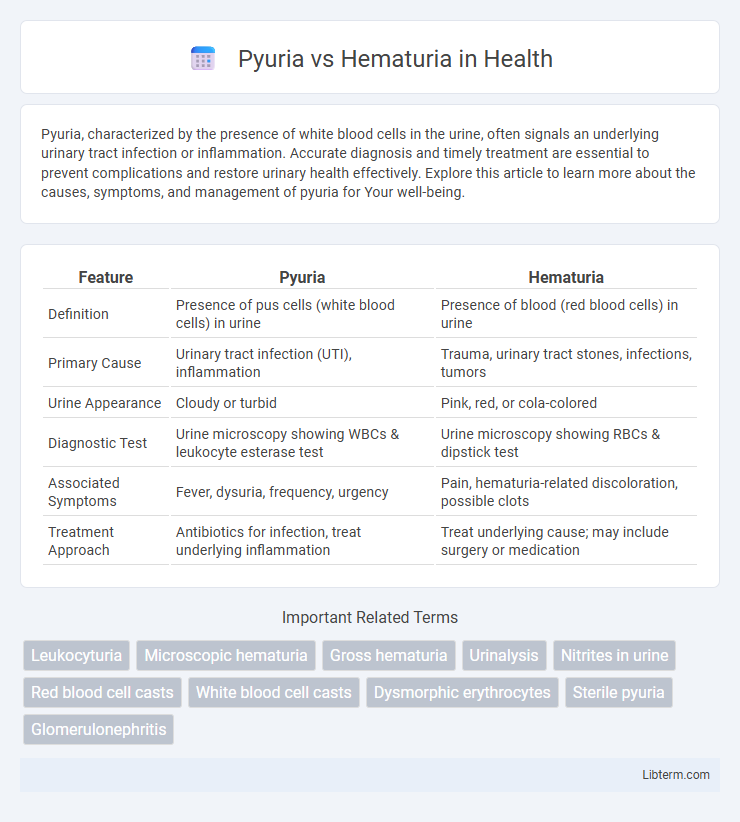
Table of Comparison
| Feature | Pyuria | Hematuria |
|---|---|---|
| Definition | Presence of pus cells (white blood cells) in urine | Presence of blood (red blood cells) in urine |
| Primary Cause | Urinary tract infection (UTI), inflammation | Trauma, urinary tract stones, infections, tumors |
| Urine Appearance | Cloudy or turbid | Pink, red, or cola-colored |
| Diagnostic Test | Urine microscopy showing WBCs & leukocyte esterase test | Urine microscopy showing RBCs & dipstick test |
| Associated Symptoms | Fever, dysuria, frequency, urgency | Pain, hematuria-related discoloration, possible clots |
| Treatment Approach | Antibiotics for infection, treat underlying inflammation | Treat underlying cause; may include surgery or medication |
Introduction to Pyuria and Hematuria
Pyuria refers to the presence of pus cells or white blood cells in the urine, typically indicating a urinary tract infection or inflammation. Hematuria is characterized by the presence of red blood cells in the urine, which may suggest urinary tract injury, infection, or malignancy. Both conditions serve as important diagnostic markers in evaluating urinary tract disorders.
Defining Pyuria: Causes and Clinical Significance
Pyuria is characterized by the presence of white blood cells in the urine, typically indicating a urinary tract infection (UTI), inflammation, or kidney disease. Common causes include bacterial infections such as cystitis and pyelonephritis, as well as non-infectious conditions like interstitial nephritis and urinary tract stones. Clinically, pyuria is a key diagnostic marker for infections and inflammation, often prompting further evaluation and targeted treatment to prevent renal complications.
Hematuria Explained: Types and Risk Factors
Hematuria refers to the presence of blood in the urine, classified into gross hematuria, where blood is visible to the naked eye, and microscopic hematuria, detected only under a microscope. Common risk factors for hematuria include urinary tract infections, kidney stones, trauma, vigorous exercise, and underlying conditions such as glomerulonephritis and bladder cancer. Early identification of hematuria types and associated risk factors is crucial for accurate diagnosis and effective management to prevent potential complications.
Key Differences Between Pyuria and Hematuria
Pyuria is characterized by the presence of white blood cells in the urine, indicating an infection or inflammation in the urinary tract, whereas hematuria involves red blood cells in the urine, suggesting bleeding or injury within the urinary system. Diagnostic measures for pyuria typically include urine microscopy showing leukocytes, while hematuria diagnosis relies on detecting erythrocytes and may require imaging to identify underlying causes. Pyuria often signals urinary tract infections like cystitis, whereas hematuria can be linked to conditions such as kidney stones, tumors, or trauma.
Common Symptoms Associated with Pyuria and Hematuria
Pyuria commonly presents with symptoms such as dysuria, urinary frequency, and lower abdominal pain, often indicating a urinary tract infection or inflammation. Hematuria typically manifests as visible blood in the urine, which may be accompanied by flank pain or signs of kidney or bladder pathology. Both conditions require diagnostic evaluation through urinalysis to differentiate between infectious, inflammatory, or structural causes.
Diagnostic Approaches for Pyuria vs Hematuria
Diagnostic approaches for pyuria prioritize urinalysis to detect leukocytes indicating urinary tract infection or inflammation, often supplemented by urine culture to identify causative pathogens. Hematuria diagnosis involves microscopic examination of urine for red blood cells, alongside imaging studies such as ultrasound or CT urography to identify structural abnormalities or malignancies in the urinary tract. Both conditions require distinct laboratory tests and imaging techniques to accurately differentiate underlying etiologies and guide appropriate clinical management.
Underlying Medical Conditions Linked to Pyuria
Pyuria, characterized by the presence of white blood cells in urine, commonly indicates urinary tract infections, kidney infections, or inflammation such as interstitial nephritis. Hematuria, defined by red blood cells in urine, often relates to conditions like urinary tract stones, trauma, or malignancies in the urinary system. Accurate differentiation between pyuria and hematuria is essential to diagnose underlying disorders such as bacterial cystitis for pyuria or glomerulonephritis associated with hematuria.
Potential Health Issues Behind Hematuria
Hematuria, the presence of blood in the urine, can indicate serious underlying health issues such as urinary tract infections, kidney stones, or even bladder cancer. Unlike pyuria, which signifies white blood cells in the urine typically due to infection or inflammation, hematuria specifically points to bleeding within the urinary system. Prompt medical evaluation is essential to diagnose conditions like glomerulonephritis, trauma, or malignancies that may cause hematuria.
Treatment Strategies for Pyuria and Hematuria
Treatment strategies for pyuria primarily involve addressing the underlying infection, typically with targeted antibiotic therapy based on urine culture sensitivity. Hematuria management depends on its cause, ranging from conservative monitoring in benign cases to interventions such as cystoscopy or surgery for structural abnormalities, tumors, or trauma. Both conditions require accurate diagnosis through urinalysis and imaging to guide appropriate and effective treatment.
Prevention and Prognosis: Managing Urinary Abnormalities
Effective prevention of pyuria and hematuria involves maintaining proper hydration, practicing good hygiene, and promptly treating urinary tract infections to reduce the risk of underlying complications. Early diagnosis and appropriate management of the root causes, such as infections, kidney stones, or trauma, significantly improve prognosis and reduce the likelihood of chronic kidney damage or recurrent urinary issues. Regular monitoring and follow-up with urinalysis help detect persistent abnormalities, guiding timely interventions and optimizing long-term urinary tract health.
Pyuria Infographic
 libterm.com
libterm.com