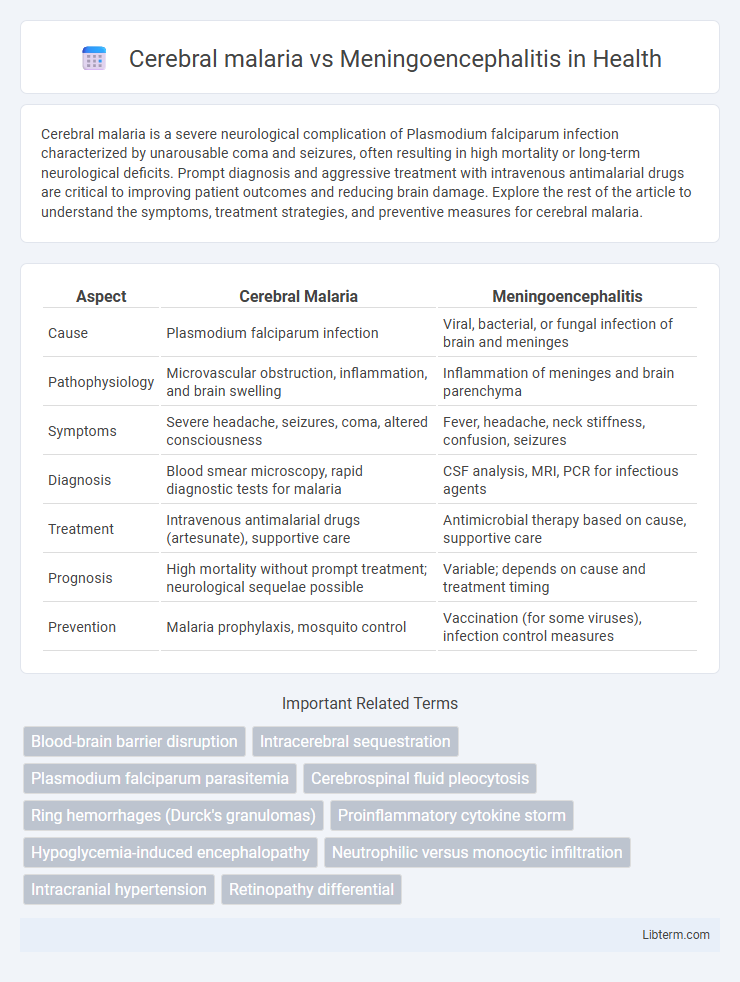
Cerebral malaria is a severe neurological complication of Plasmodium falciparum infection characterized by unarousable coma and seizures, often resulting in high mortality or long-term neurological deficits. Prompt diagnosis and aggressive treatment with intravenous antimalarial drugs are critical to improving patient outcomes and reducing brain damage. Explore the rest of the article to understand the symptoms, treatment strategies, and preventive measures for cerebral malaria.
Table of Comparison
| Aspect | Cerebral Malaria | Meningoencephalitis |
|---|---|---|
| Cause | Plasmodium falciparum infection | Viral, bacterial, or fungal infection of brain and meninges |
| Pathophysiology | Microvascular obstruction, inflammation, and brain swelling | Inflammation of meninges and brain parenchyma |
| Symptoms | Severe headache, seizures, coma, altered consciousness | Fever, headache, neck stiffness, confusion, seizures |
| Diagnosis | Blood smear microscopy, rapid diagnostic tests for malaria | CSF analysis, MRI, PCR for infectious agents |
| Treatment | Intravenous antimalarial drugs (artesunate), supportive care | Antimicrobial therapy based on cause, supportive care |
| Prognosis | High mortality without prompt treatment; neurological sequelae possible | Variable; depends on cause and treatment timing |
| Prevention | Malaria prophylaxis, mosquito control | Vaccination (for some viruses), infection control measures |
Introduction to Cerebral Malaria and Meningoencephalitis
Cerebral malaria is a severe neurological complication of Plasmodium falciparum infection characterized by impaired consciousness and seizures due to parasitized red blood cells obstructing cerebral microvasculature. Meningoencephalitis involves inflammation of the brain and meninges caused by infectious agents such as viruses, bacteria, or fungi, leading to symptoms like headache, fever, and altered mental status. Differentiating cerebral malaria from meningoencephalitis relies on clinical presentation, laboratory tests including blood smears for malaria parasites, and neuroimaging findings to guide appropriate treatment.
Etiology: Key Causes and Risk Factors
Cerebral malaria is caused by Plasmodium falciparum infection transmitted through Anopheles mosquito bites, with risk factors including living in or traveling to endemic tropical regions, especially sub-Saharan Africa. Meningoencephalitis arises from viral, bacterial, fungal, or parasitic infections, such as herpes simplex virus, Neisseria meningitidis, or Cryptococcus neoformans, with immunocompromised status and exposure to infectious agents as significant risk factors. Both conditions exhibit distinct pathogen etiologies and are influenced by geographic, environmental, and host immune factors.
Pathophysiological Differences
Cerebral malaria is caused by Plasmodium falciparum infection, leading to microvascular obstruction due to sequestration of parasitized red blood cells in cerebral capillaries, resulting in impaired blood flow, hypoxia, and brain edema. Meningoencephalitis involves inflammation of both the meninges and brain parenchyma, typically triggered by viral or bacterial pathogens that induce an immune-mediated response causing neuronal injury and increased blood-brain barrier permeability. The primary pathophysiological distinction lies in cerebral malaria's vascular occlusion and hypoxic injury versus meningoencephalitis' inflammatory infiltration and immune-mediated neuronal damage.
Epidemiological Overview and Geographic Distribution
Cerebral malaria primarily affects sub-Saharan Africa, accounting for the highest morbidity and mortality rates among children under five, with Plasmodium falciparum as the main causative agent. Meningoencephalitis shows a more diverse geographic distribution, prevalent in regions where specific viral, bacterial, or fungal pathogens are endemic, including parts of Asia, Europe, and the Americas. Epidemiological data highlight that cerebral malaria cases peak during rainy seasons due to increased mosquito vector activity, whereas meningoencephalitis incidence correlates with pathogen-specific outbreaks and seasonal factors depending on the etiology.
Clinical Presentation: Signs and Symptoms
Cerebral malaria presents with sudden onset of high fever, severe headache, confusion, seizures, and altered consciousness, often progressing rapidly to coma. Meningoencephalitis features symptoms such as fever, neck stiffness, photophobia, headache, seizures, and altered mental status, reflecting inflammation of both the brain and meninges. Both conditions share neurological deficits and seizures, but cerebral malaria typically includes systemic signs of severe malaria like anemia and jaundice, while meningoencephalitis often follows infectious etiologies like viral or bacterial pathogens.
Diagnostic Modalities: Tests and Criteria
Cerebral malaria diagnosis relies on identifying Plasmodium falciparum parasites through peripheral blood smears, rapid diagnostic tests (RDTs), and clinical criteria such as unarousable coma with no other cause. Meningoencephalitis diagnostic modalities include cerebrospinal fluid (CSF) analysis via lumbar puncture, revealing elevated white cell count, increased protein, and sometimes pathogen-specific PCR assays. Neuroimaging like MRI or CT scans aids in distinguishing cerebral malaria's diffuse brain swelling from meningoencephalitis focal lesions or edema patterns.
Treatment Approaches and Therapeutic Guidelines
Treatment approaches for cerebral malaria emphasize rapid administration of intravenous artesunate followed by a full course of oral artemisinin-based combination therapy (ACT) to reduce parasitic load and prevent neurological damage. In contrast, meningoencephalitis management varies with etiology, often requiring empirical intravenous broad-spectrum antibiotics such as ceftriaxone and antivirals like acyclovir until specific pathogens are identified via CSF analysis. Therapeutic guidelines for cerebral malaria prioritize supportive care including seizure control and management of increased intracranial pressure, whereas meningoencephalitis protocols focus on tailored antimicrobial therapy and adjunctive corticosteroids, particularly in bacterial cases, to minimize inflammation and neurological sequelae.
Prognosis and Complication Profiles
Cerebral malaria, caused by Plasmodium falciparum infection, typically presents a worse prognosis due to high mortality rates and frequent neurological sequelae such as cognitive impairment and motor deficits. In contrast, meningoencephalitis, often resulting from viral or bacterial infections, shows variable prognosis depending on the pathogen and timeliness of treatment, with complications including seizures, hydrocephalus, and lasting neurocognitive dysfunction. Both conditions require urgent medical intervention, but cerebral malaria's complications tend to be more severe and life-threatening, emphasizing the need for rapid diagnosis and intensive care.
Preventive Strategies and Public Health Implications
Preventive strategies for cerebral malaria rely heavily on vector control measures such as insecticide-treated bed nets, indoor residual spraying, and prompt antimalarial treatment, targeting Plasmodium falciparum transmission in endemic regions. Meningoencephalitis prevention focuses on vaccination programs against common causative pathogens like Neisseria meningitidis, Haemophilus influenzae type b, and viral agents, combined with public health education on hygiene and early symptom recognition. Both conditions demand robust surveillance systems and community awareness campaigns to reduce incidence, morbidity, and mortality, emphasizing integrated approaches tailored to regional epidemiology and healthcare infrastructure.
Summary: Key Differences and Clinical Implications
Cerebral malaria is a severe neurological complication of Plasmodium falciparum infection characterized by coma and seizures, whereas meningoencephalitis involves inflammation of the brain and meninges due to viral or bacterial infections. Key differences include etiology--parasitic versus infectious agents--and clinical presentation, where cerebral malaria often presents with retinopathy and rapid neurological deterioration. Understanding these distinctions is critical for timely diagnosis and appropriate treatment strategies, as cerebral malaria requires antimalarial therapy while meningoencephalitis demands targeted antimicrobial management.
Cerebral malaria Infographic
 libterm.com
libterm.com