Peptic ulcer disease causes painful sores in the lining of your stomach or the upper part of your small intestine, often resulting from Helicobacter pylori infection or prolonged use of NSAIDs. Key symptoms include burning stomach pain, bloating, and nausea, which can significantly impact your daily comfort and health. Discover effective treatments, lifestyle changes, and prevention tips by reading the rest of this article.
Table of Comparison
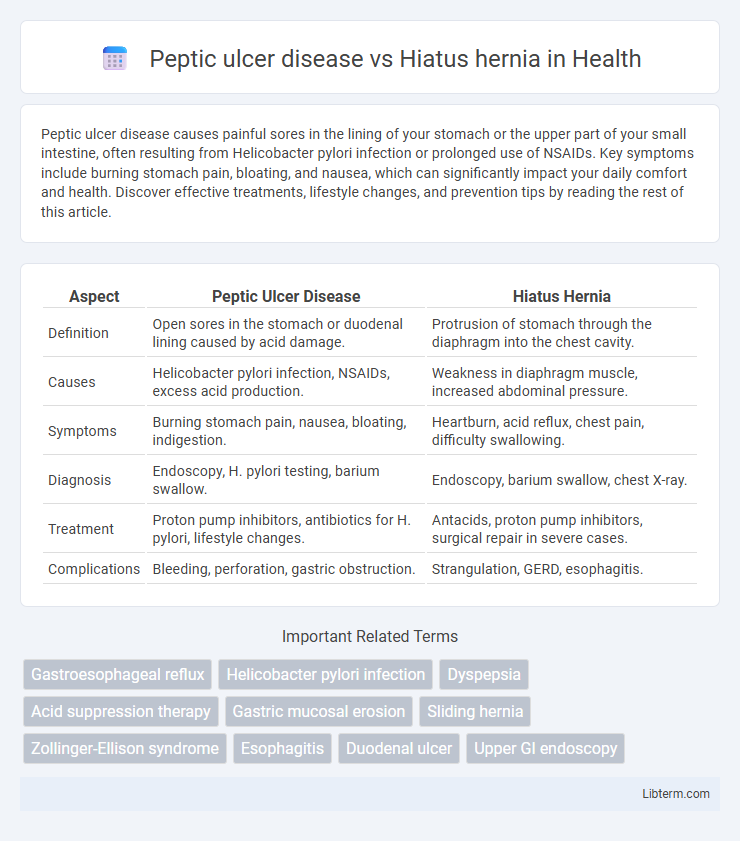
| Aspect | Peptic Ulcer Disease | Hiatus Hernia |
|---|---|---|
| Definition | Open sores in the stomach or duodenal lining caused by acid damage. | Protrusion of stomach through the diaphragm into the chest cavity. |
| Causes | Helicobacter pylori infection, NSAIDs, excess acid production. | Weakness in diaphragm muscle, increased abdominal pressure. |
| Symptoms | Burning stomach pain, nausea, bloating, indigestion. | Heartburn, acid reflux, chest pain, difficulty swallowing. |
| Diagnosis | Endoscopy, H. pylori testing, barium swallow. | Endoscopy, barium swallow, chest X-ray. |
| Treatment | Proton pump inhibitors, antibiotics for H. pylori, lifestyle changes. | Antacids, proton pump inhibitors, surgical repair in severe cases. |
| Complications | Bleeding, perforation, gastric obstruction. | Strangulation, GERD, esophagitis. |
Introduction to Peptic Ulcer Disease and Hiatus Hernia
Peptic ulcer disease involves the formation of painful sores or ulcers in the lining of the stomach or the first part of the small intestine due to acid damage, commonly caused by Helicobacter pylori infection or long-term use of NSAIDs. Hiatus hernia occurs when part of the stomach protrudes through the diaphragm into the chest cavity, often leading to gastroesophageal reflux symptoms. Both conditions affect the upper gastrointestinal tract but differ significantly in pathophysiology, symptoms, and treatment approaches.
Definition and Overview
Peptic ulcer disease (PUD) is characterized by open sores that develop on the inner lining of the stomach, duodenum, or esophagus due to the corrosive effects of stomach acid and Helicobacter pylori infection. Hiatus hernia occurs when part of the stomach protrudes through the diaphragm into the chest cavity, often causing gastroesophageal reflux symptoms. Both conditions affect the upper gastrointestinal tract but differ fundamentally in their anatomical disruption and underlying pathophysiology.
Epidemiology and Prevalence
Peptic ulcer disease (PUD) affects approximately 10% of the global population with higher prevalence in regions with Helicobacter pylori infection rates exceeding 50%, predominantly in developing countries. Hiatus hernia is reported in up to 60% of individuals over 50 years old, with increased incidence linked to obesity and aging populations in developed nations. Epidemiological data indicate PUD incidence has decreased due to effective H. pylori eradication, whereas hiatus hernia prevalence rises with lifestyle factors and demographic shifts.
Causes and Risk Factors
Peptic ulcer disease primarily results from Helicobacter pylori infection and prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs), with risk factors including smoking, excessive alcohol consumption, and chronic stress. Hiatus hernia occurs due to weakening of the diaphragm muscle or increased intra-abdominal pressure, often linked to obesity, aging, and persistent coughing or heavy lifting. Both conditions are influenced by lifestyle factors, but peptic ulcers are more closely associated with gastric acid secretion and bacterial infection, whereas hiatus hernia involves anatomical displacement of the stomach through the esophageal hiatus.
Pathophysiology: Peptic Ulcer Disease vs Hiatus Hernia
Peptic ulcer disease arises from the disruption of the gastric or duodenal mucosal barrier due to excessive gastric acid secretion and Helicobacter pylori infection, leading to localized mucosal erosion. In contrast, a hiatus hernia results from the protrusion of the stomach through the diaphragmatic esophageal hiatus, causing mechanical disruption and impaired lower esophageal sphincter function. While peptic ulcers primarily involve mucosal injury driven by acid-pepsin imbalance, hiatus hernia pathophysiology centers on anatomical displacement causing gastroesophageal reflux and associated esophageal irritation.
Clinical Manifestations and Symptoms
Peptic ulcer disease typically presents with gnawing or burning epigastric pain that often improves with food intake but worsens a few hours after meals, accompanied by nausea, bloating, and occasional melena or hematemesis in severe cases. Hiatus hernia commonly causes gastroesophageal reflux symptoms such as heartburn, regurgitation, and chest discomfort, with some patients experiencing dysphagia or chronic cough due to acid irritation. While both conditions involve upper gastrointestinal discomfort, peptic ulcer pain is more localized and related to acid secretion, whereas hiatus hernia mainly results in reflux-related symptoms caused by anatomical disruption of the gastroesophageal junction.
Diagnostic Approaches
Peptic ulcer disease diagnosis relies primarily on endoscopy to visualize ulcers and biopsy for Helicobacter pylori infection, with urea breath tests and stool antigen tests confirming H. pylori presence. Hiatus hernia diagnosis typically involves barium swallow radiography and upper endoscopy to identify the herniation of the stomach into the thoracic cavity. Esophageal manometry and pH monitoring may be used to assess associated gastroesophageal reflux in hiatus hernia cases.
Complications and Long-Term Outcomes
Peptic ulcer disease complications include bleeding, perforation, and gastric outlet obstruction, which can lead to peritonitis and sepsis if untreated. Hiatus hernia complications primarily involve gastroesophageal reflux disease (GERD), esophagitis, and in severe cases, strangulation of the herniated stomach portion causing ischemia. Long-term outcomes for peptic ulcer disease depend on controlling Helicobacter pylori infection and acid suppression, whereas hiatus hernia management focuses on mitigating reflux symptoms and preventing esophageal strictures or Barrett's esophagus.
Treatment Strategies and Management
Treatment strategies for peptic ulcer disease primarily involve eradication of Helicobacter pylori infection using a combination of antibiotics and proton pump inhibitors (PPIs) to reduce gastric acid secretion and promote healing. Management of hiatus hernia focuses on lifestyle modifications such as weight loss and dietary changes, alongside pharmacologic therapy with antacids, H2-receptor antagonists, or PPIs to control gastroesophageal reflux symptoms. In severe cases of hiatus hernia, surgical intervention like Nissen fundoplication may be indicated, contrasting with peptic ulcer disease where surgery is reserved for complications such as perforation or bleeding.
Prevention and Lifestyle Modifications
Peptic ulcer disease prevention focuses on reducing Helicobacter pylori infection risk, avoiding NSAIDs, limiting alcohol intake, and managing stress to promote gastric mucosal healing. Hiatus hernia prevention emphasizes weight management, avoiding heavy lifting, quitting smoking, and implementing dietary changes to reduce acid reflux and intra-abdominal pressure. Adopting a balanced diet rich in fiber, practicing portion control, and maintaining an upright posture after meals play critical roles in managing both conditions effectively.
Peptic ulcer disease Infographic
 libterm.com
libterm.com