Facility-acquired infections pose significant risks to patient safety and can lead to extended hospital stays and increased healthcare costs. Understanding the common sources and preventive measures is crucial for minimizing these infections and ensuring better health outcomes. Explore the rest of the article to learn how you can protect yourself and others from facility-acquired infections.
Table of Comparison
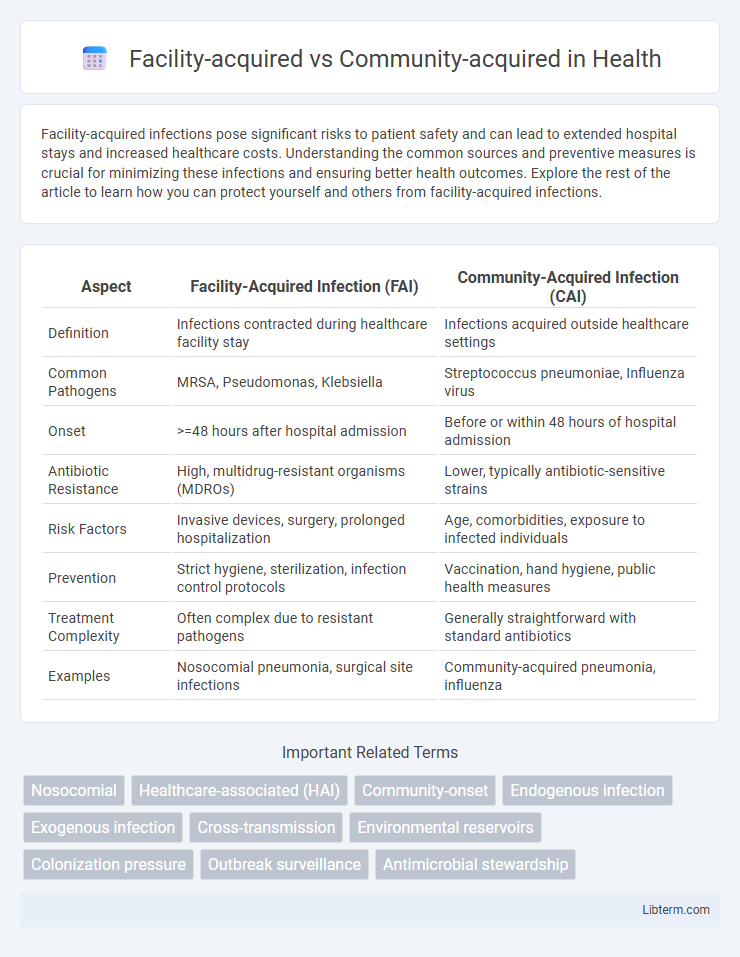
| Aspect | Facility-Acquired Infection (FAI) | Community-Acquired Infection (CAI) |
|---|---|---|
| Definition | Infections contracted during healthcare facility stay | Infections acquired outside healthcare settings |
| Common Pathogens | MRSA, Pseudomonas, Klebsiella | Streptococcus pneumoniae, Influenza virus |
| Onset | >=48 hours after hospital admission | Before or within 48 hours of hospital admission |
| Antibiotic Resistance | High, multidrug-resistant organisms (MDROs) | Lower, typically antibiotic-sensitive strains |
| Risk Factors | Invasive devices, surgery, prolonged hospitalization | Age, comorbidities, exposure to infected individuals |
| Prevention | Strict hygiene, sterilization, infection control protocols | Vaccination, hand hygiene, public health measures |
| Treatment Complexity | Often complex due to resistant pathogens | Generally straightforward with standard antibiotics |
| Examples | Nosocomial pneumonia, surgical site infections | Community-acquired pneumonia, influenza |
Introduction to Facility-Acquired vs Community-Acquired Infections
Facility-acquired infections (FAIs), also known as healthcare-associated infections (HAIs), occur in patients during their stay in healthcare settings such as hospitals or nursing homes, typically developing 48 hours or more after admission. Community-acquired infections (CAIs) are contracted outside healthcare environments and are present or incubating at the time of admission. Understanding the distinctions between FAIs and CAIs is critical for infection control strategies and guiding appropriate antimicrobial treatment.
Key Definitions and Terminology
Facility-acquired infections develop within healthcare settings such as hospitals or long-term care facilities, typically manifesting 48 hours or more after admission, indicating transmission within the facility. Community-acquired infections are contracted outside healthcare environments, present or incubating at the time of admission, often linked to environmental exposure or person-to-person contact. Understanding the distinction involves terms like nosocomial infections (synonymous with facility-acquired) and incubation period, which is critical for accurate diagnosis and epidemiological tracking.
Sources and Transmission Pathways
Facility-acquired infections primarily originate from invasive procedures, contaminated medical equipment, and healthcare workers' hands, with transmission pathways including direct contact, droplet spread, and environmental reservoirs within hospital settings. Community-acquired infections typically arise from person-to-person contact, respiratory droplets, and contaminated surfaces in public or household environments. Understanding these distinct sources and transmission routes is crucial for implementing targeted infection control strategies.
Common Types of Facility-Acquired Infections
Facility-acquired infections commonly include catheter-associated urinary tract infections (CAUTIs), central line-associated bloodstream infections (CLABSIs), surgical site infections (SSIs), and ventilator-associated pneumonia (VAP), reflecting the high-risk environments within hospitals and long-term care facilities. These infections arise due to invasive procedures, prolonged hospital stays, and the presence of multidrug-resistant organisms, contrasting with community-acquired infections that often involve respiratory or gastrointestinal pathogens. Effective infection control measures in healthcare settings target reducing device-related infections and improving hand hygiene to minimize facility-acquired infection rates.
Common Types of Community-Acquired Infections
Common types of community-acquired infections include respiratory infections like influenza and community-acquired pneumonia, skin infections such as cellulitis and impetigo, and gastrointestinal infections caused by pathogens like norovirus and Salmonella. These infections typically occur outside healthcare settings and are often transmitted through close contact, contaminated food or water, and respiratory droplets. Understanding pathogen prevalence and antibiotic resistance patterns in community settings is crucial for effective treatment and prevention strategies.
Risk Factors and Vulnerable Populations
Facility-acquired infections primarily affect patients with prolonged hospital stays, invasive procedures, or weakened immune systems, such as those in intensive care units or with chronic illnesses. Community-acquired infections often impact individuals with increased exposure to crowded environments, poor sanitation, or pre-existing conditions like diabetes and asthma. Vulnerable populations for both types include elderly adults, immunocompromised individuals, and patients with comorbidities, highlighting the need for targeted prevention strategies in healthcare and community settings.
Diagnostic Differences
Facility-acquired infections often require more advanced diagnostic approaches, including molecular testing and culture techniques, to identify multidrug-resistant organisms prevalent in healthcare settings. Community-acquired infections typically rely on rapid antigen detection tests and routine cultures due to the lower likelihood of resistant pathogens. Differentiating the infection source guides appropriate antimicrobial stewardship and infection control practices.
Treatment Approaches and Management
Facility-acquired infections often require aggressive antibiotic regimens due to multidrug-resistant organisms frequently encountered in healthcare settings, emphasizing the need for targeted antimicrobial stewardship programs. Community-acquired infections typically respond to standard empiric therapies based on local susceptibility patterns, with management focusing on early diagnosis and outpatient care when appropriate. Infection control protocols and patient monitoring differ significantly, with facility-acquired cases demanding stringent isolation measures and multidisciplinary management to prevent transmission and complications.
Prevention Strategies and Best Practices
Facility-acquired infections require stringent infection control protocols, including hand hygiene compliance, environmental cleaning, and antibiotic stewardship to prevent multidrug-resistant organisms. Community-acquired infections emphasize vaccination programs, public health education, and early detection to reduce transmission outside healthcare settings. Implementing targeted screening and isolation strategies in healthcare facilities further minimizes the spread of pathogens and improves patient outcomes.
Conclusion and Future Directions
Facility-acquired infections often present with higher antibiotic resistance compared to community-acquired cases, necessitating tailored antimicrobial stewardship strategies. Emphasizing rapid diagnostic tools and enhanced infection control protocols can significantly reduce transmission within healthcare settings. Future research should prioritize genomic surveillance and personalized treatment approaches to improve patient outcomes across both environments.
Facility-acquired Infographic
 libterm.com
libterm.com