Biliary colic causes intense abdominal pain due to gallstones blocking the bile duct, often triggered by fatty meals. Understanding the symptoms and treatment options can help prevent complications like cholecystitis or pancreatitis. Explore this article to learn how you can manage biliary colic effectively and recognize when to seek medical help.
Table of Comparison
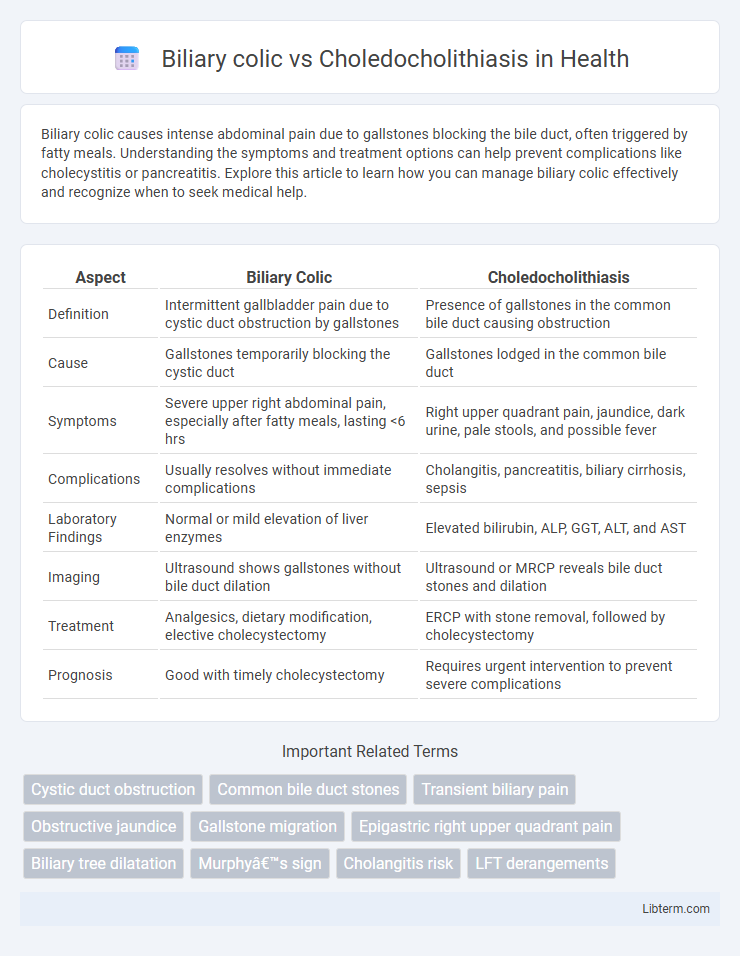
| Aspect | Biliary Colic | Choledocholithiasis |
|---|---|---|
| Definition | Intermittent gallbladder pain due to cystic duct obstruction by gallstones | Presence of gallstones in the common bile duct causing obstruction |
| Cause | Gallstones temporarily blocking the cystic duct | Gallstones lodged in the common bile duct |
| Symptoms | Severe upper right abdominal pain, especially after fatty meals, lasting <6 hrs | Right upper quadrant pain, jaundice, dark urine, pale stools, and possible fever |
| Complications | Usually resolves without immediate complications | Cholangitis, pancreatitis, biliary cirrhosis, sepsis |
| Laboratory Findings | Normal or mild elevation of liver enzymes | Elevated bilirubin, ALP, GGT, ALT, and AST |
| Imaging | Ultrasound shows gallstones without bile duct dilation | Ultrasound or MRCP reveals bile duct stones and dilation |
| Treatment | Analgesics, dietary modification, elective cholecystectomy | ERCP with stone removal, followed by cholecystectomy |
| Prognosis | Good with timely cholecystectomy | Requires urgent intervention to prevent severe complications |
Introduction to Biliary Colic and Choledocholithiasis
Biliary colic arises from the temporary obstruction of the cystic duct by gallstones, causing intense, intermittent right upper quadrant pain often triggered by fatty meals. Choledocholithiasis involves the presence of gallstones in the common bile duct, leading to bile flow obstruction, jaundice, and potential complications like cholangitis or pancreatitis. Differentiating these conditions is crucial since choledocholithiasis typically requires more invasive intervention compared to the often self-limiting biliary colic.
Definition and Pathophysiology
Biliary colic is defined as episodic, severe pain caused by temporary obstruction of the cystic duct by gallstones, leading to increased pressure in the gallbladder. Choledocholithiasis involves the presence of gallstones in the common bile duct, resulting in bile flow obstruction and potential complications such as cholangitis or pancreatitis. The pathophysiology of biliary colic centers on transient gallbladder distension and smooth muscle spasm, whereas choledocholithiasis causes prolonged ductal obstruction, inflammation, and possible bile duct infection.
Causes and Risk Factors
Biliary colic is primarily caused by transient obstruction of the cystic duct due to gallstones, while choledocholithiasis results from stones lodged in the common bile duct, often originating from the gallbladder. Risk factors for both conditions include obesity, female gender, age over 40, rapid weight loss, and certain genetic predispositions affecting cholesterol metabolism. In choledocholithiasis, additional risks include previous gallbladder surgery and biliary tract infections that promote stone formation in the bile ducts.
Clinical Presentation and Symptoms
Biliary colic typically presents with sudden, severe right upper quadrant abdominal pain often radiating to the right shoulder or back, accompanied by nausea and vomiting, but usually without fever or jaundice. Choledocholithiasis manifests with similar abdominal pain but is frequently accompanied by jaundice, dark urine, pale stools, and possible fever, indicating biliary obstruction and cholangitis. Laboratory findings in choledocholithiasis often show elevated bilirubin, alkaline phosphatase, and transaminases, distinguishing it from uncomplicated biliary colic.
Diagnostic Approaches and Imaging
Ultrasound is the first-line imaging modality for diagnosing biliary colic, revealing gallstones and gallbladder wall thickening without bile duct dilation. Magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EUS) are more sensitive for detecting choledocholithiasis, identifying stones within the common bile duct and assessing ductal dilation. Laboratory tests combined with imaging findings, such as elevated liver function tests and bilirubin levels, support the diagnosis and guide further interventions like endoscopic retrograde cholangiopancreatography (ERCP).
Laboratory Findings and Interpretation
Biliary colic typically presents with normal liver function tests, as the gallbladder obstruction is transient and does not cause bile duct inflammation, whereas choledocholithiasis often shows elevated bilirubin, alkaline phosphatase, and gamma-glutamyl transferase levels due to biliary obstruction and cholestasis. Elevated serum transaminases (AST and ALT) may be mild in biliary colic but are usually more pronounced in choledocholithiasis when accompanied by cholangitis or hepatic injury. Amylase and lipase levels may increase in choledocholithiasis complicated by pancreatitis, distinguishing it from uncomplicated biliary colic.
Key Differences Between Biliary Colic and Choledocholithiasis
Biliary colic primarily involves transient obstruction of the cystic duct by gallstones, causing episodic right upper quadrant pain without infection or jaundice. Choledocholithiasis refers to the presence of stones in the common bile duct, often leading to persistent pain, jaundice, abnormal liver function tests, and a higher risk of cholangitis or pancreatitis. Imaging modalities such as ultrasound and MRCP are essential for differentiating biliary colic from choledocholithiasis by identifying stone location and ductal dilation.
Complications and Associated Conditions
Biliary colic primarily involves transient obstruction of the cystic duct by gallstones, often leading to intense right upper quadrant pain without infection, but repeated episodes can cause gallbladder inflammation or cholecystitis. Choledocholithiasis, characterized by gallstones in the common bile duct, carries higher risks of serious complications including cholangitis, pancreatitis, and obstructive jaundice due to bile duct obstruction and bacterial infection. Both conditions are associated with gallstone disease, but choledocholithiasis necessitates prompt intervention to prevent life-threatening sepsis and biliary cirrhosis.
Management and Treatment Options
Biliary colic is managed primarily with pain control using NSAIDs or opioids and often requires elective laparoscopic cholecystectomy to prevent recurrence, while acute episodes necessitate fasting and hydration. Choledocholithiasis treatment involves urgent endoscopic retrograde cholangiopancreatography (ERCP) to remove common bile duct stones, followed by cholecystectomy to reduce the risk of complications such as cholangitis or pancreatitis. Supportive care includes intravenous fluids, antibiotics if infection is present, and monitoring for signs of biliary obstruction or sepsis.
Prognosis and Patient Outcomes
Biliary colic typically has a favorable prognosis with resolution following the passage or removal of gallstones, often without long-term complications. Choledocholithiasis carries a higher risk of severe outcomes, including biliary obstruction, cholangitis, and pancreatitis, necessitating timely intervention to prevent morbidity and mortality. Early detection and management are crucial in choledocholithiasis to improve patient outcomes and reduce the likelihood of recurrent biliary events.
Biliary colic Infographic
 libterm.com
libterm.com